
It includes 13 modules, 5 CPD hours, and self-accreditation with the RANZCP and RACGP.
Start learning today:
@psychscene.bsky.social
We provide psychiatry education for Psychiatrists, GPs & Mental Health Practitioners.

It includes 13 modules, 5 CPD hours, and self-accreditation with the RANZCP and RACGP.
Start learning today:
In this course, you will learn how to:
-Explain key features and impacts of melancholic and psychotic depression
-Accurately diagnose both conditions
-Discuss treatment and management options
-Diagnose major depressive disorder with mixed features (DMX)

This curriculum offers diagnostic clarity and management strategies for melancholic, psychotic, and mixed-feature depression.
15.11.2025 07:23 — 👍 0 🔁 0 💬 1 📌 0
This advanced on-demand course led by Dr Sanil Rege builds on foundational formulation skills and transitions toward translating diagnostic insights into targeted management strategies.
Enroll now:

Here’s what your colleague has to say about our course: “The Art of Strategic Problem Solving in Psychiatry – From Diagnostic Formulation to Management”:
08.11.2025 14:09 — 👍 0 🔁 0 💬 1 📌 0
For an in-depth learning on diagnoses of anxiety and other mental disorders, visit The Academy
Summary of Assessment Approach
Is it Anxiety?
Is the Anxiety Severe?
Is it an Anxiety Disorder?
Does it meet the criteria for GAD, PD, or SAD?
Use Clinical Practice Guidelines to plan treatment.
Consider other diagnoses and appropriate referral when necessary.
Medical Contributors to Rule Out
Substance-induced (intoxication, withdrawal, caffeine)
Medical Conditions (hyperthyroidism, seizures, hypoglycaemia)
Differentiate from MDD
MDD: primary low mood/anhedonia with past-oriented rumination (“Why did I…”) plus hopelessness.
GAD: primary anxiety with future-oriented “what if…”, prominent muscle tension, and secondary low mood.
Differentiate from OCD
OCD has circumscribed, unwanted intrusive thoughts with compulsions and harm/contamination themes; thoughts feel alien and are ritual-neutralised.
GAD worries are internally congruent, everyday, predominantly verbal, and not ritual-driven.
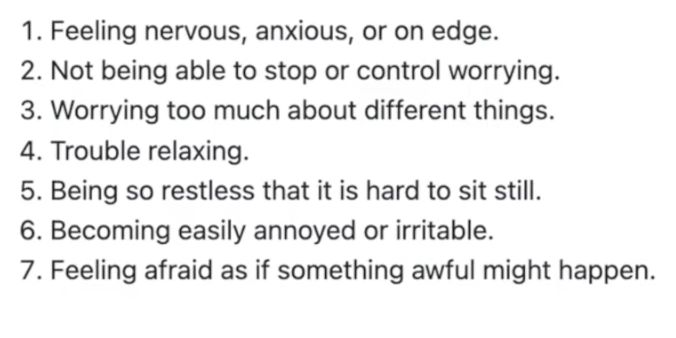
GAD-7 Self-Assessment
This diagnostic tool detects a patient’s latent anxiety.
These items are answered by frequency (not at all, most days, etc.)
[Spitzer et al., 2006]
Diagnostic Interview
“Are you a worrier?”
“How long each day do worries occupy you?”
“What do you worry about?””
Probe tension headaches/neck tightness, sleep onset/maintenance, concentration, avoidance, and functional impact.

DSM-5 anchors you can count.
Excessive worry more days than not for ≥6 months about multiple domains, difficult to control.
Plus ≥3 of restlessness, fatigue, poor concentration/mind blank, irritability, muscle tension, and sleep disturbance.
Nature of Anxiety.
Worry is frequent, excessive, hard to switch off, and out of keeping with threat, often without a trigger.
It persists even when things are going well and becomes the problem, not the topic [Andrews et al., 2018].

Chelsea, 20, says she’s “going mad with anxiety.”
Onset with VCE exams; now pervasive worry, decision paralysis, and no depressive features.
You suspect GAD.
What would you do to confirm this? 👇

Want to go deeper into the diagnosis and complexities of ADHD?
Join Dr. Sanil Rege for the ADHD Masterclass: From Neurobiology to Clinical Practice on the 29th of November:
Psych Scene Tip
When assessing females:
• Ask beyond classroom disruption, explore internal experiences.
• Adapt rating scales (e.g., “excessive giggling/talking” vs. aggression).
• Screen for comorbidities and masking behaviours.
(Young et al., 2020)
Underdiagnosis may lead to higher risks of:
• Depression and anxiety
• Eating disorders
• Substance use
• Relationship and occupational impairment
Early recognition changes lifelong trajectories.
Females with ADHD may present with:
• Inattention, disorganisation, overwhelm
• Emotional dysregulation
• Fatigue and low motivation
• Co-occurring anxiety or mood disorders
Hyperactivity is less visible but often internal, restlessness, racing thoughts, impulsive decisions
Hormonal Influences
Hormones modulate dopamine and serotonin systems.
Oestrogen increases dopamine receptor density, improving focus, while low-oestrogen phases (premenstrual, postpartum, menopause) can exacerbate ADHD symptoms.
The Female Protective Effect
Females may require a higher threshold of genetic or environmental stressors for ADHD to manifest.
This “protective effect” delays recognition, until academic or social transitions reveal underlying difficulties.
Neurodevelopmental Differences
Brain maturation differs between sexes.
Females reach total cerebral volume ~4 years earlier (Lenroot et al., 2007), influencing symptom timing and diagnosis.
Cross-sectional studies may misinterpret these developmental differences as absence of pathology.
Compared to boys, girls with ADHD show:
• More emotional lability
• Higher anxiety and mood symptoms
• Greater risk of being bullied
• Stronger prosocial behaviours
These features often hide underlying ADHD. (Nøvik et al., 2006)
Girls tend to compensate through compliance, social adaptability, and resilience.
They internalise distress rather than externalising it, leading to misdiagnosis as anxiety, depression, or personality disorders.
Girls often present with inattentive rather than disruptive symptoms.
They may appear dreamy, disorganised, or emotionally sensitive, not “hyperactive.”
These traits are less likely to trigger referral or concern.
ADHD is diagnosed far more often in males than females.
Early studies show teachers are more likely to refer boys for assessment, even when girls show identical symptoms. (Young et al., 2020)

Females with ADHD are often underdiagnosed and undertreated, forming a silent minority.
Research shows a significant male-to-female diagnosis gap (Berry et al., 1985).
Let’s explore why ADHD presents differently in females.

Want to go deeper into the diagnosis and complexities of ADHD?
Join Dr. Sanil Rege for the ADHD Masterclass: From Neurobiology to Clinical Practice on the 29th of November:
Psych Scene Tip
When assessing females:
• Ask beyond classroom disruption, explore internal experiences.
• Adapt rating scales (e.g., “excessive giggling/talking” vs. aggression).
• Screen for comorbidities and masking behaviours.
(Young et al., 2020)
Underdiagnosis may lead to higher risks of:
• Depression and anxiety
• Eating disorders
• Substance use
• Relationship and occupational impairment
Early recognition changes lifelong trajectories.