This post hoc analysis of the subgroup of patients with P. aeruginosa BSI recruited for the BALANCE RCT showed no differences in 90d mortality between patients treated for 7 vs 14d.
However, sample size and wide CIs preclude definite conclusions.
academic.oup.com/cid/advance-... #IDsky #AMSsky
05.03.2026 08:42 —
👍 4
🔁 1
💬 0
📌 0

El 18 de Marzo celebramos en Sevilla la IX Jornada de TB celebrando el día mundial de la TB. La inscripción es gratuita. Será presencial y on line simultáneamente. Os animamos a participar
#Tuberculosis #TBSky
28.02.2026 12:30 —
👍 1
🔁 1
💬 0
📌 0
ClinicalTrials.gov
Stay tuned
TAPER V2
Vanco taper Vs Fidaxomicin
Vancomycin Taper to Prevent Recurrent Clostridioides Difficile (TAPER-V2)
Study Details | NCT07328971 | Vancomycin Taper to Prevent Recurrent Clostridioides Difficile | #Idsky
clinicaltrials.gov/study/NCT07328…
27.02.2026 22:06 —
👍 1
🔁 1
💬 0
📌 0

Promotional Toolkit
ESCMID Global (formerly ECCMID): an annual congress bringing together experts and specialists in Clinical Microbiology and Infectious Diseases.
With ESCMID Global quickly approaching!
To help you spread the word and get involved, check out ESCMID Global 2026 Promotional Toolkit
The official hashtag for the congress this year is #ESCMIDGlobal2026 on all social media channels. #IDSky
www.escmid.org/congress-eve...
13.02.2026 17:30 —
👍 5
🔁 4
💬 0
📌 0

Panel A: The weekly Gravitrap Aedes aegypti index (GAI), which measures the abundance of adult A. aegypti mosquitoes, in the intervention and control clusters before and during the release of wolbachia-infected male mosquitoes.
Panel B: A spatial visualization of the intervention (red) and control (teal) clusters.
In this report from Singapore, the release of wolbachia-infected, irradiated male 𝘈𝘦𝘥𝘦𝘴 𝘢𝘦𝘨𝘺𝘱𝘵𝘪 mosquitoes resulted in a reduction in the vector population and in the risk of dengue infection. Full report: nej.md/4atd2iN
#MedSky #IDSky
11.02.2026 22:25 —
👍 24
🔁 10
💬 1
📌 3

An illustrated diagram of the immunopathophysiology of VITT.
VITT is caused by a somatic hypermutation of an anti–adenovirus pVII antibody that generates more avid binding of platelet factor 4 than of adenovirus pVII, its original target, which results in platelet activation. Full study results: nej.md/3MBnaOx
#MedSky #Hematology
11.02.2026 23:01 —
👍 15
🔁 3
💬 0
📌 0

Advantages with HD. Check out this week’s KASIC pearl to learn about Hemodialysis-only Antibiotic Dosing kymdro.org/kasic/?p=8784
#IDsky #AntimicrobialResistance #antimicrobialstewardship #rxsky #pharmacy #FOAMed #NPs #PAs
17.01.2026 15:26 —
👍 3
🔁 3
💬 0
📌 0
Non pay walled link: authors.elsevier.com/a/1mCdH3AjoX...
07.12.2025 03:32 —
👍 6
🔁 2
💬 1
📌 1

Clarity Initiative
Clinical Literature Appraisal and Research education in InfecTious diseases
A group of ID clinical researchers passionate about clinical research and evidence appraisal has just launched the CLARITY initiative (clarityinitiative.org), which aims to improve the generation and interpretation of evidence in ID and Microbiology.
30.11.2025 23:39 —
👍 17
🔁 11
💬 1
📌 0
En infección urinaria, menos es más 👌🏻
Nuestro hilo sobre diagnóstico y tratamiento de la infección urinaria.
☝🏻 Bacteriuria asintomática
#EAAD #WAAW #AMSsky #MedSky #UTIsky
(🧵1/2)
bsky.app/profile/hosp...
24.11.2025 22:33 —
👍 2
🔁 1
💬 1
📌 0
👆🏻 #AMSsky
20.11.2025 00:17 —
👍 0
🔁 0
💬 0
📌 0

💡Applications for the 2026-2028 AMS Certificate Programme & EUCIC Certificate Programme are open! These training programmes are designed to strengthen your expertise in antimicrobial stewardship & IPC.
Learn more:
AMS: https://ow.ly/kYz550Xu6iW
EUCIC: https://ow.ly/zlsl50Xu6iU
#IDSky #clinmicro
19.11.2025 16:05 —
👍 0
🔁 2
💬 1
📌 0
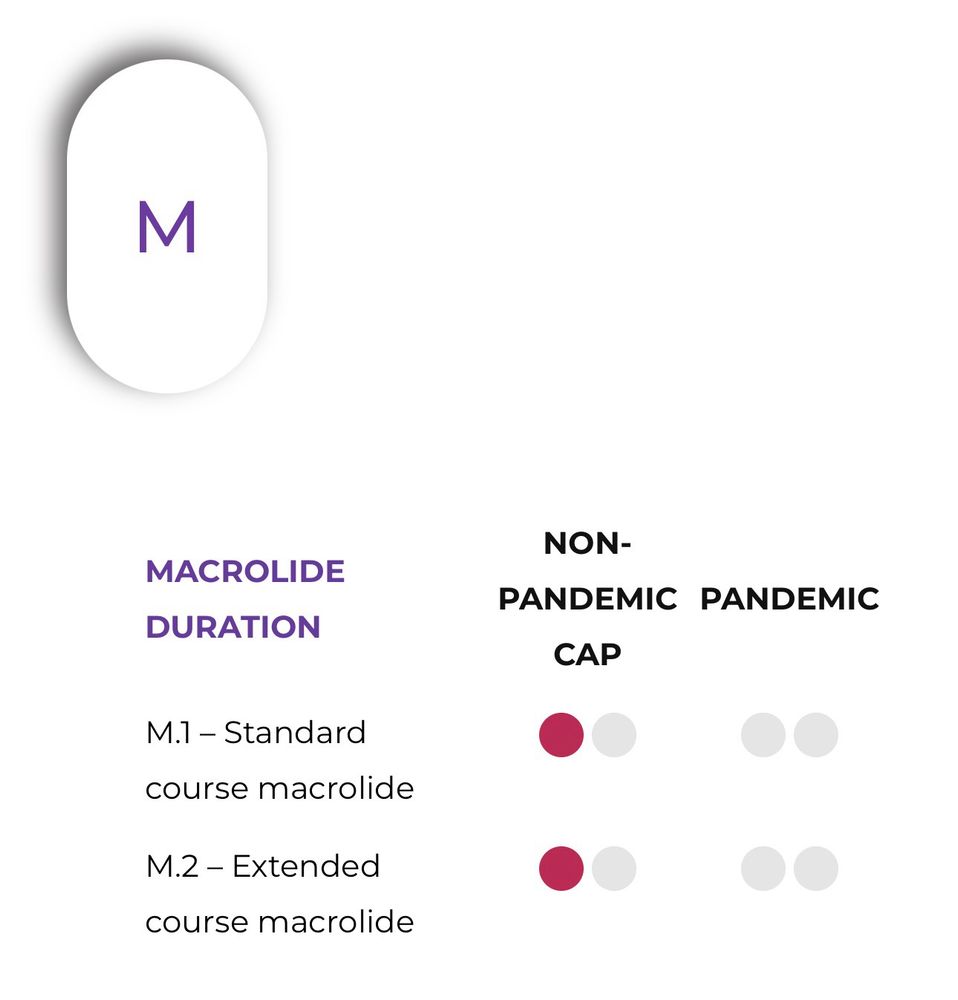
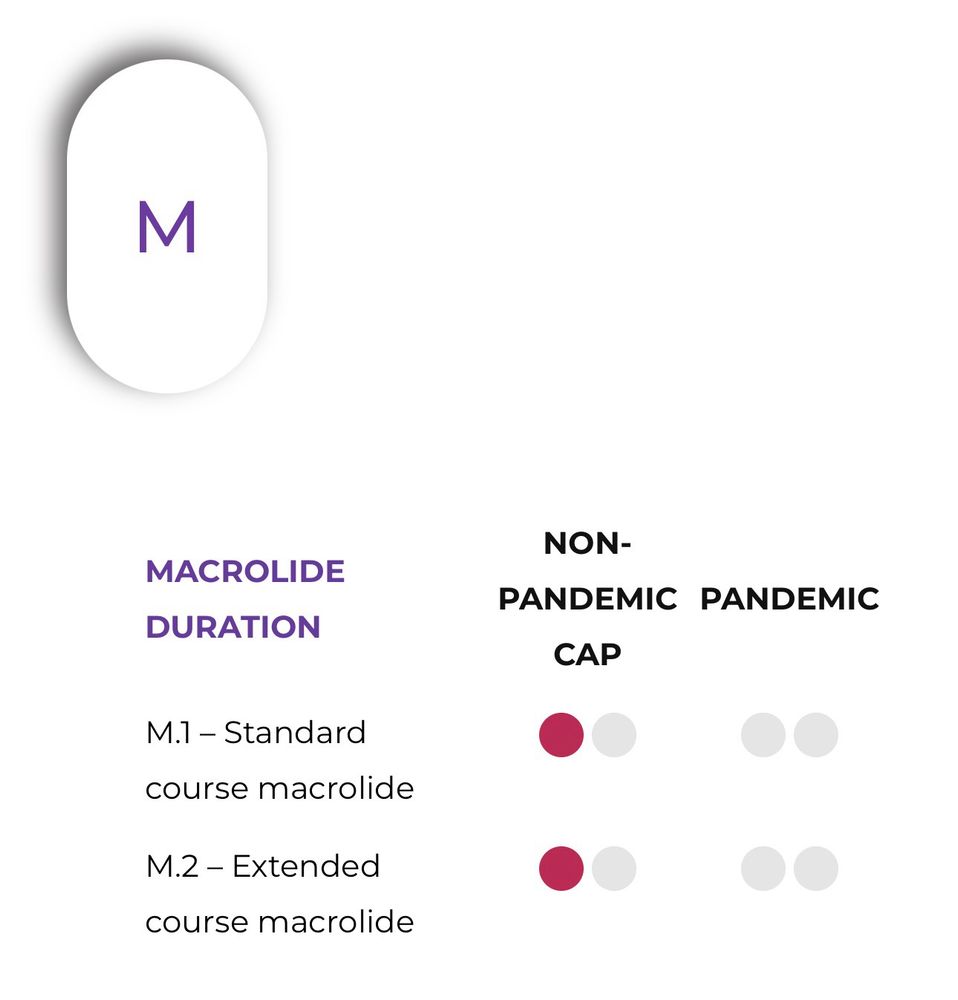
#WinterIsComing 🥶
Un hilo con nuestras recomendaciones para acertar con tus tratamientos de consulta para las infecciones respiratorias.
☝🏻 Neumonías y EPOC reagudizado
#EAAD #WAAW #AMSsky #MedSky #PharmSky
(🧵1/4)
bsky.app/profile/hosp...
19.11.2025 19:37 —
👍 2
🔁 1
💬 1
📌 0
¿Trabajas en consulta?
¡Te necesitamos!
El uso prudente de los antibióticos es responsabilidad de todos. Durante toda esta semana, no te pierdas nuestros vídeos para hacer un uso prudente de los antibióticos.
💪🏻 ¡La lucha contra las resistencias empieza en tu consulta!
#EAAD #WAAW #AMSsky
18.11.2025 20:34 —
👍 2
🔁 2
💬 1
📌 1

¿Trabajas en consulta?
¡Te necesitamos!
Durante toda esta semana, no te pierdas nuestra serie de vídeos prácticos para hacer un uso prudente de los antibióticos en tus pacientes ambulatorios
👊🏻 La lucha contra las resistencias, empieza en tu consulta
#EAAD #WAAW #AMSsky #MedSky #PharmSky #SomosHUVR
18.11.2025 07:54 —
👍 5
🔁 3
💬 1
📌 0

¡Ya tenemos todo listo para el Día Europeo para el Uso Prudente de los Antibióticos!
Mantente atento a las redes de @hospitaluvrocio.bsky.social y @guiaprioam.bsky.social durante la semana que viene.
Tenemos un mensaje para ti… 😉
#EAAD #WAAW #AMSsky #SomosHUVR
13.11.2025 09:36 —
👍 5
🔁 2
💬 0
📌 0
It’s SO #AMSsky… 😂😂😂
22.10.2025 14:32 —
👍 3
🔁 0
💬 0
📌 0

Dr Tamma mentions the ongoing GOAT trial (PI Tamma & Cosgrove)
This will be a most needed and important study. clinicaltrials.gov/study/NCT060...
#IDweek2025 #IDsky
19.10.2025 18:46 —
👍 19
🔁 4
💬 1
📌 1

New from IDSA, thanks to Dr William Werbel, resp virus vax in immunocompromised population:
- vax 2 weeks before or 3-6 months after immunocompromise expected
- expect blunted response if given within that window
- defer during acute rejection, illness
- adjust for viral circulation
#IDSky #IDWeek
20.10.2025 19:06 —
👍 8
🔁 3
💬 1
📌 1
Fantastic - this will be an impactful study on treatment duration of blood stream Pseudomonas infection.
Our centre already mostly does 7 days (and my prediction is that this will be non-inferior) but it's RCT like these that will shift dial across the board with persuasive evidence.
#IDSky #AMR
18.10.2025 11:37 —
👍 15
🔁 5
💬 1
📌 0
The rationale of the RCT was testing the current standard (7d) in the specific setting of Pseudomonas BSIs.
The DURATIONS design is a relevant contribution, but it adds complexity and I wonder if a multi-arm (5?) approach is convenient when testing durations in such a narrow timeframe.
19.10.2025 05:53 —
👍 2
🔁 0
💬 1
📌 0
There was a session at ESCMID 2025 on macrolides for CAP and this paper was heavily featured (lead investigator was panelist). Patient population in this trial was much “sicker” than in other studies. I was convinced of their role and benefit, but not for every hospitalized pt (icu only perhaps)
18.10.2025 13:26 —
👍 3
🔁 1
💬 1
📌 0

Totally agree. Definitely not for any CAP.
I was also shocked by the mean age (>80y) and Charlson. Probably this was a major driver for the high mortality, beyond the severity of the infection itself — mean CURB65 was 2-3, the setting for recruitment were Internal Medicine wards instead of ICUs…
18.10.2025 17:18 —
👍 1
🔁 0
💬 1
📌 0

I have the same concern!
In this RCT, 25% of patients received steroids in both arms.
The subgroup analysis showed benefits independently (and apparently superior) to the use of steroids, but this relevant question was not primarily addressed by the trial
pdf.sciencedirectassets.com/271247/1-s2....
18.10.2025 16:58 —
👍 2
🔁 0
💬 0
📌 0

Full protocol: https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0277333
Recruitment for SHORTEN-2 is officially complete!
Our team is now wrapping up follow-up and polishing databases. Hope to have results ready in the first half of 2026!
Hats off to this awesome research team! 🥳
#AMSsky #IDsky @seimc.bsky.social @ciberisciii.bsky.social @ibis-investigacion.bsky.social
18.10.2025 09:57 —
👍 15
🔁 6
💬 0
📌 1

I think REMAP-CAP has ongoing domains to adress this question, hopefully we’ll get new data soon to confirm the hypothesis
🤞🏻 www.remapcap.eu/domains/
18.10.2025 09:18 —
👍 1
🔁 0
💬 1
📌 0