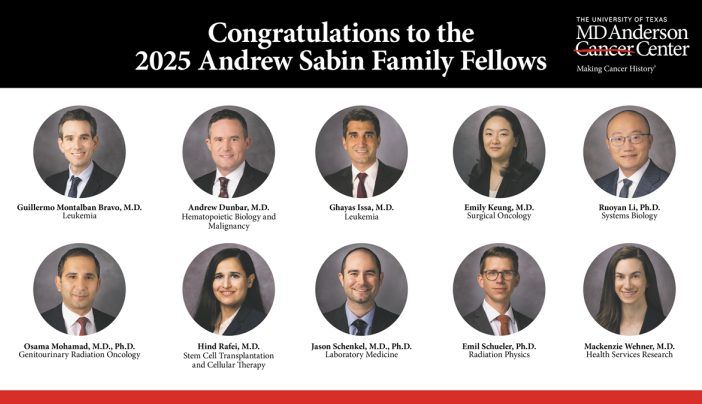
Thrilled to be honored as one of the 2026 Young Physician Scientist Awards from the @the-asci.org! Looking forward to being back in my old stomping grounds in Chicago!!! @mdanderson.bsky.social
20.01.2026 22:51 — 👍 5 🔁 1 💬 1 📌 0
I am grateful to have trained at such an incredible center during my graduate school years. Marc’s contributions at the helm of the CFI cannot be understated. Thank you Marc, for your service and leadership!
25.08.2025 14:21 — 👍 0 🔁 0 💬 0 📌 0

With deep gratitude, we thank Dr. Marc Jenkins for his decades of leadership, mentorship, and dedication to the Center for Immunology. The foundation he built will guide and inspire us for years to come.
25.08.2025 12:06 — 👍 16 🔁 6 💬 2 📌 0
Fantastic new paper looking at the extrinsic effects of PD-1 loss! Check it out.
24.07.2025 17:23 — 👍 11 🔁 1 💬 1 📌 0
Center for Immunology
Kicking off our journey on BlueSky! We're excited to share updates and connect with you. Follow us and help us get the word out! For more information about the Center for Immunology, go to our website: immunology.umn.edu
02.04.2025 18:47 — 👍 18 🔁 8 💬 1 📌 0
Excited to share this preprint: In trial led by @michaelpelusomd.bsky.social and Steve Deeks, combination immunotherapy=>high rate of HIV control (low VL) after ART pause. @demisandel.bsky.social in our lab found control associated with robust CD8+ T cell proliferation early in response to rebound.
20.03.2025 18:06 — 👍 11 🔁 5 💬 0 📌 0
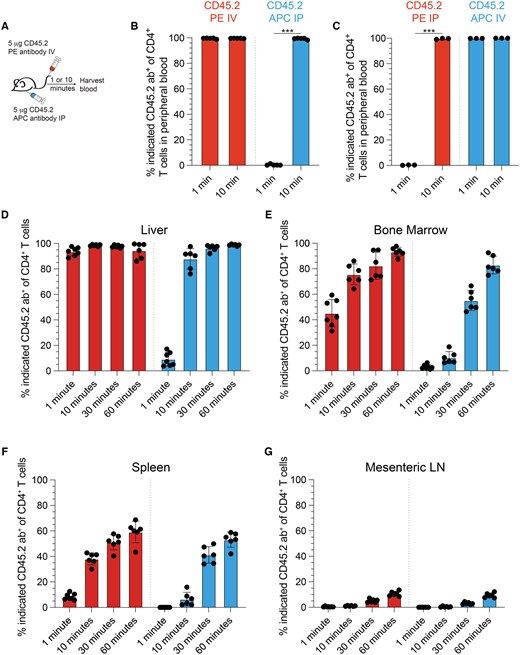
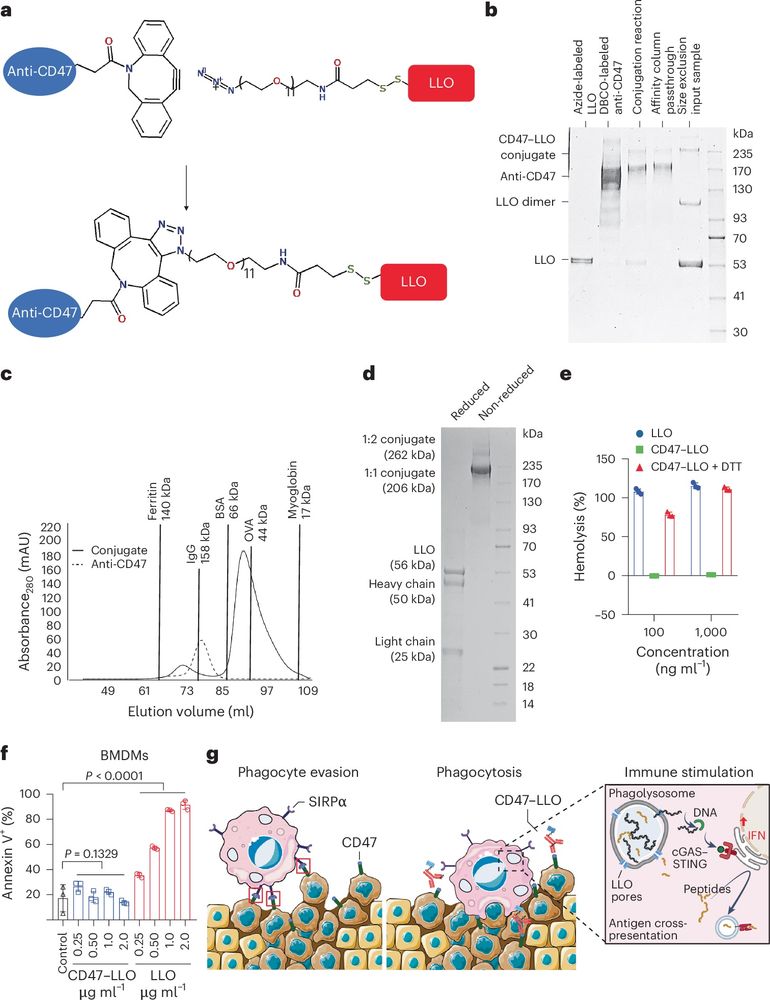
Different injection routes and fluorophores affect anti-CD45.2 antibody leukocyte labeling @jmschenkel.bsky.social @jimmunol.bsky.social @thenatcat.bsky.social
doi.org/10.1093/jimm...
13.03.2025 02:55 — 👍 4 🔁 1 💬 0 📌 0
I am very grateful for the team we have and look forward to getting the next few of these out the door! We are not done yet! Though it may be a hot minute before the next one comes out. Hopefully pre-prints soon at least! Stay tuned! 11/end
10.03.2025 11:00 — 👍 0 🔁 0 💬 0 📌 0
We believe these data will be food for thought for folks interested in using our in vivo labeling. And maybe just a fun read for folks who are lymphatic drainage enthusiasts. Big congrats to the lab for closing out our second paper! 10/n
10.03.2025 11:00 — 👍 1 🔁 1 💬 1 📌 0
In short, BB700 was the big winner. It continuously labeled for over 6 hours in vivo (crazy right???). Applying it to a transplantable tumor model, we found we could identify roughly 7-fold more tumor specific CD8s that had recently migrated compared to IV administration. 9/n
10.03.2025 11:00 — 👍 0 🔁 0 💬 1 📌 0
Because antibody could be found in the plasma for a while, we speculated we could try and find fluorophores that were capable of labeling at low concentrations. This may provide an opportunity to extend the labeling window for rare events! So that’s what we did with serial dilution experiments. 8/n
10.03.2025 11:00 — 👍 0 🔁 0 💬 1 📌 0
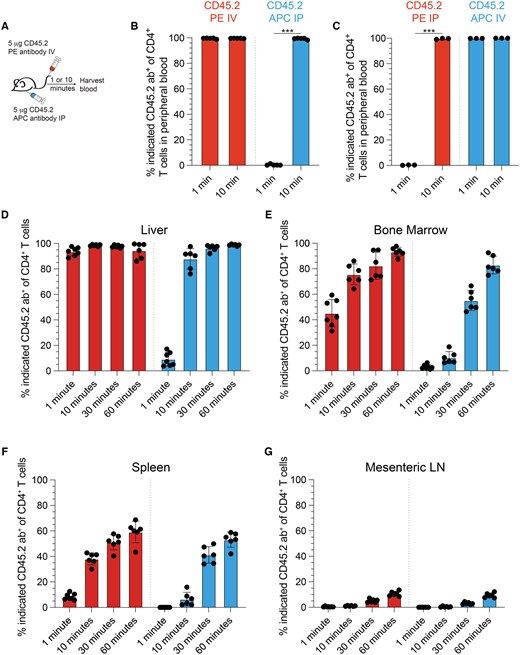
We next developed a homegrown ELISA to quantify circulating CD45.2 IV and IP antibodies. We saw that IP anti-CD45.2 concentration gradually increased over an hour, while IV disappeared. 7/n
10.03.2025 11:00 — 👍 0 🔁 0 💬 1 📌 0
Moreover, when we examined leukocyte labeling in blood contiguous compartments like the red pulp of the spleen, liver, and bone marrow, we found that IP antibody labeling intensity increased over the course of an hour, suggesting that labeling was continuously happening. 6/n
10.03.2025 11:00 — 👍 0 🔁 0 💬 1 📌 0
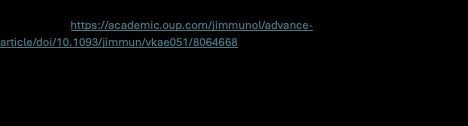
We find that IP injection of anti-CD45.2 antibody does not label cells in the blood as quickly as an IV injection (duh, I know! But still!). IV injection labels all circulating cells within a minute. Whereas we do not get full labeling by IP injection for at least 10 minutes. 5/n
10.03.2025 11:00 — 👍 0 🔁 0 💬 1 📌 0
Have you ever wondered about how injecting antibodies via intravenous (IV) or intraperitoneal (IP) injection differs? As a field, we often use IP injection for antibody treatments, and I have always found this to be interesting to think through how IP vs IV injectioun routes may be different. 3/n
10.03.2025 11:00 — 👍 0 🔁 0 💬 1 📌 0
One of our big limitations was that it was hard to track rare migration events due to a limited labeling window. More on that in a second. 2/n
10.03.2025 11:00 — 👍 0 🔁 0 💬 1 📌 0
I am pleased to announce that our newest story is officially out at @jimmunol.bsky.social ! academic.oup.com/jimmunol/adv...
This is an immediate follow up to the lab’s first paper from last year. We again thank @jimmunol.bsky.social for a smooth, efficient, and wonderfully fair review process. 1/n
10.03.2025 11:00 — 👍 6 🔁 2 💬 1 📌 0

Building Cure at the Seattle Children's Research Institute
Super excited to announce that the Joag Lab will officially open at @UW, @SCRI in March 2025! We will study the interplay between memory T cells and stromal, humoral, and innate immunity in mucosal tissues. researcherprofiles.seattlechildrens.org/Vineet.Joag. Hiring a technician and a postdoc!
22.01.2025 18:14 — 👍 15 🔁 9 💬 2 📌 0
The Journal of Immunology (@jimmunol.bsky.social)
Keep your eyes peeled for #2 (jimmunol.bsky.social). And submitted our first big kid grants. Hoping for some kindness from reviewers... Very excited to see what things will look like in another year! What a whirlwind of a job - 2 years have flown by! Feeling both lucky and privileged.
22.12.2024 22:38 — 👍 2 🔁 0 💬 1 📌 0
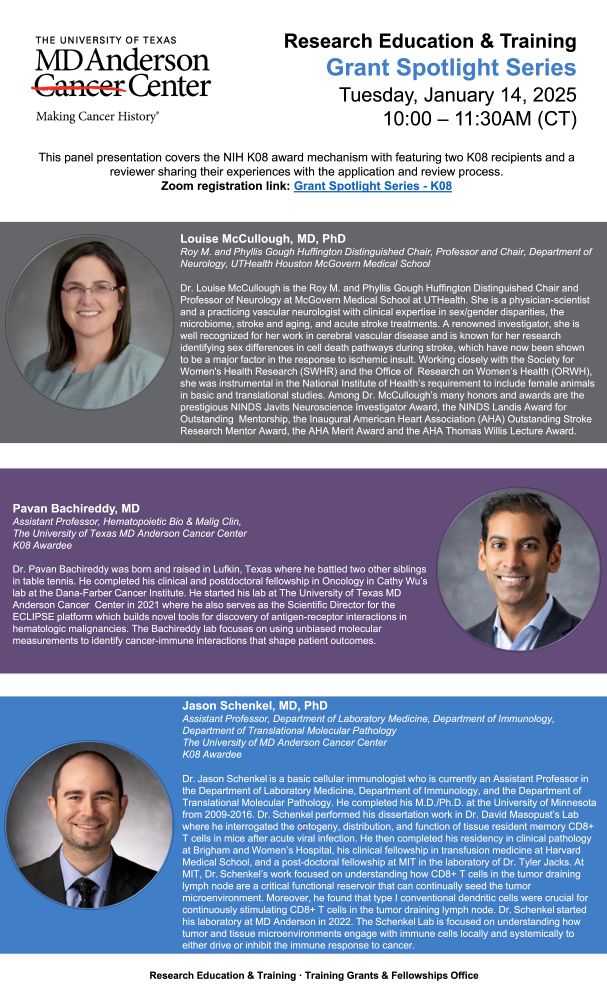
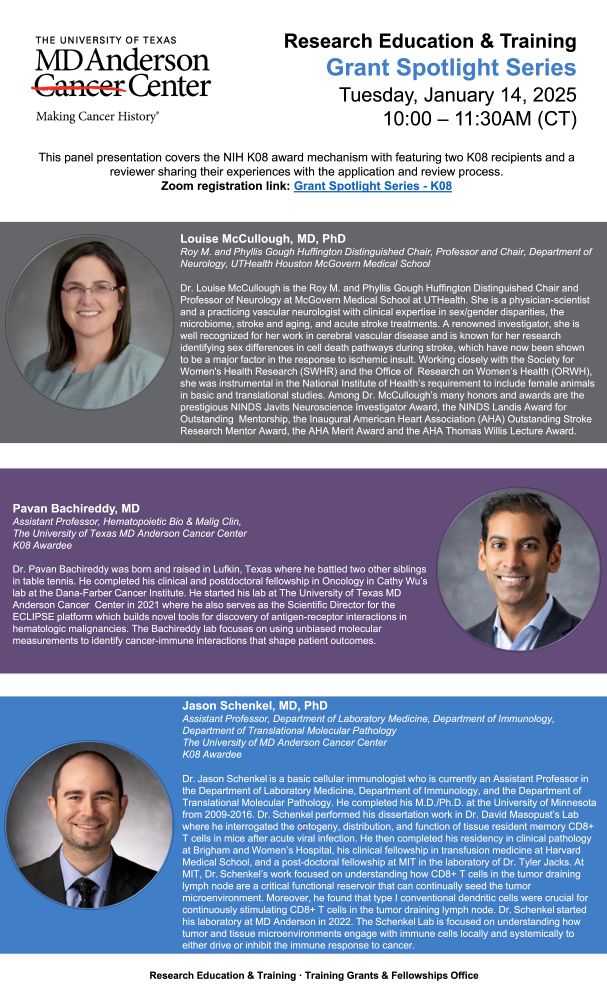
Attention physician scientists! Are you interested in applying for a K08? Of course you are! I will be part of a NIH broadcasted information session featuring myself and another K08 awardee, as well as a reviewer from a K08 study section in January. See the attached flyer! And please repost!
17.12.2024 04:08 — 👍 5 🔁 3 💬 1 📌 1
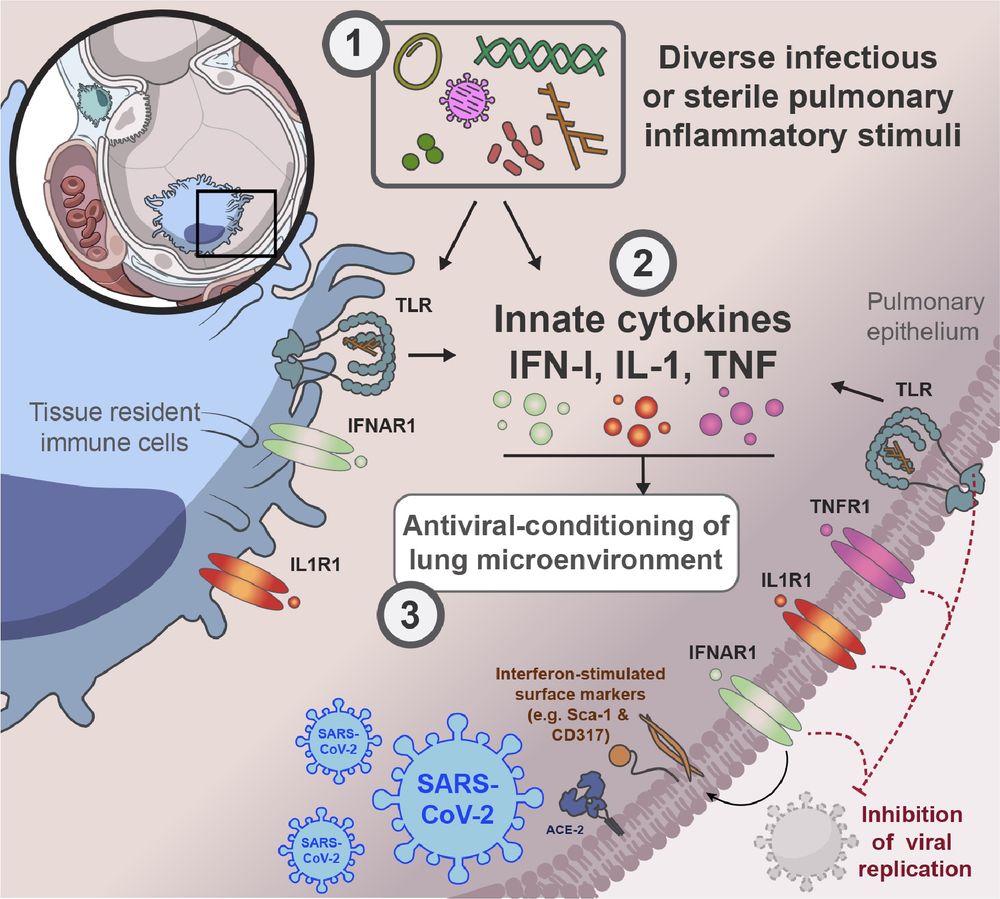
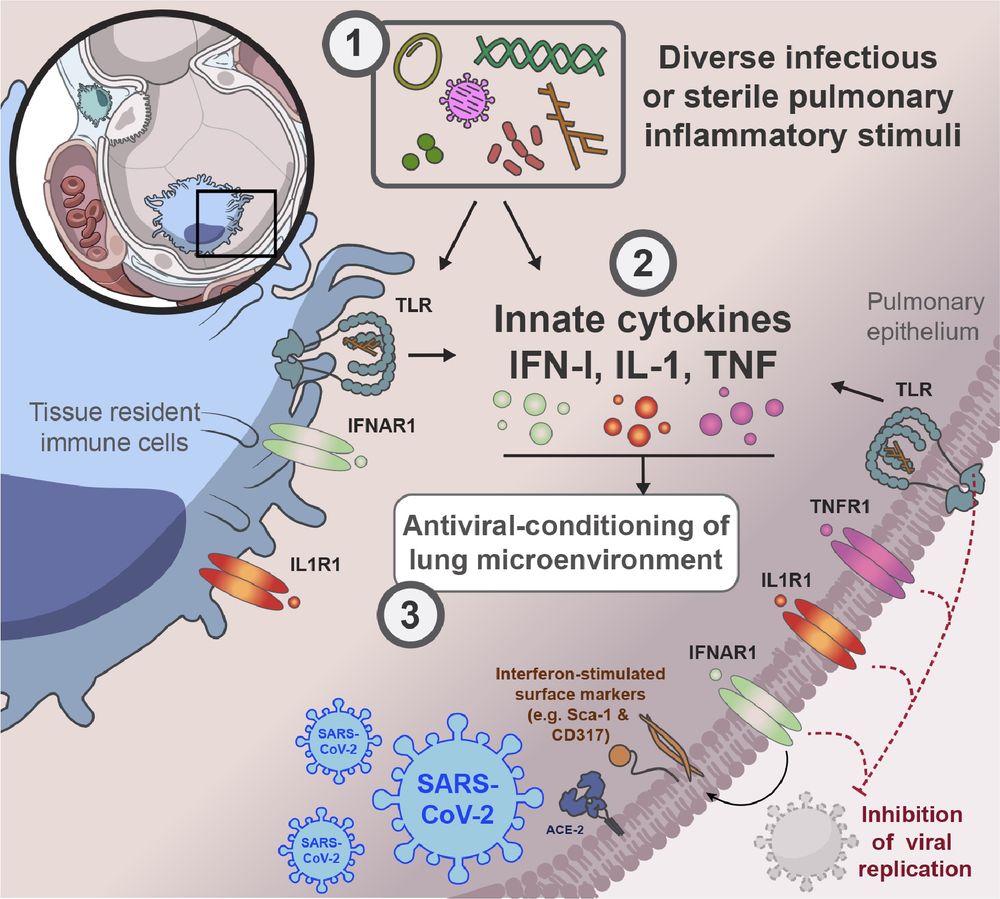
Graphical summary of our paper. In mice, prior lower airway exposure to diverse inflammatory stimuli, including chronic bacterial infections such as M. tuberculosis, acute bacterial infections such as pulmonary S. aureus, viral infections such as Influenza A, type-II allergic responses such as the OVA-Alum model, activation of pulmonary TLR9 by CpG or pulmonary TLR1/2 by Pam3CSK4
leads to reduced viral burden upon subsequent infection with SARS-CoV-2 (SCV2). (2) This SCV2 restriction occurs prior to induction of SCV2-specific adaptive immune responses
and is mediated through innate immune responses, including the induction of IFN-I, TNFα and IL-1 and sustained changes to the TRM (Tissue resident macrophage) cellular
compartment and the pulmonary epithelium. (3) Innate cytokine and TLR signaling to both recruited immune cells and the pulmonary epithelium creates a microenvironment in the
lung that limits early replication of SCV2. IFN-I signaling to pulmonary ECs (epithelial cells) increases expression of interferon-stimulated genes, that likely cell-intrinsically limit viral
replication. TNF- or IL-1 suppress SCV2 independently of IFN-I signaling. TNF acts exclusively through radio-resistant cell types such as the lung epithelium, whereas IL-1 affords
control both direct and indirectly, through either stromal and hematopoietic cell types, to restrict overall early SCV2 burden.
Best #Nikolaus 🎅! Our paper on how the 🫁 microenvironment can shape #innate immunity against #viruses is out @sciimmunology.bsky.social This was a herculean effort brilliantly led by @pauljbaker.bsky.social who singlehandedly established the model in the lab during the pandemic. 🧪 #Immunosky 1/9
06.12.2024 22:37 — 👍 296 🔁 84 💬 28 📌 9
Sing Sing Way at Cincinnati Children’s is a great scientist and collaborator!
02.12.2024 00:14 — 👍 2 🔁 0 💬 0 📌 0
The ASCI is a nonprofit honor society of physician-scientists. Founded in 1908, the Society is home to 3,500+ members across academic medicine and industry.
https://the-asci.org
Take action for federal funding of research:
https://www.fundresearch.org/
We are the Withers lab, based at the @oxcio.bsky.social at the Nuffield Department of Medicine, Oxford.
Our research is focused upon understanding how immune cells adapt to, and are changed by tissues, particularly the tumour microenvironment.
Assistant Member/Professor, Lab Head @MSKCancerCenter. #PhysicianScientist #Immunologist. Views my own.
Physician-scientist in training. Neurologist. The Reich lab. NIH/NINDS. Interested in neuroscience, immunology, neurology, math and physics. Opinions are my own.
https://scholar.google.com/citations?hl=en&user=8HkrbWkAAAAJ&view_op=list_works
Post doc fellow, Zon lab, Harvard. PhD, Weizmann Institute, Israel. A firm believer that the zebrafish natural habitat is under a very good microscope.
The Immunological Genome Project (ImmGen) is a collaborative group of immunology and computational biology labs who join forces and expertise to perform a broad and deep dissection of the genome’s activity and its regulation in the murine immune system.
Immunology PhD Candidate | Vanderbilt University | passionate about T cells & tumor immunology
INM – Leibniz Institute for New Materials is a research institute in Saarland, Germany that is exploring new materials for a better world
leibniz-inm.de/en/imprint/
Study genetic conflicts professionally. Try to avoid conflicts in personal life (with mixed results).
Fred Hutch Basic Sciences,
UW Genome Sciences,
HHMI.
Posting in a personal capacity. My posts don’t reflect my employers’ opinions.
🔬 Assistant Prof, Pathology @Duke | Director, Clin Micro Lab
🧫 Former Clin Micro Fellow @Memorial Sloan Kettering
👩🏻🔬 Former Postdoc @broadinstitute.org
🎓 PhD @The Rockefeller University
Focus: Diagnostics, AMR, Structural Biology
4x father - infectious diseases specialist with scientific interest in tuberculosis, HIV and the host response - book nerd.
Professional sceptic; never heard an uninteresting fact about T cells; I like microorganisms/microbiomes too.
Human B cell responses to emerging pathogens 🦠
Icahn School of Medicine at Mount Sinai, NYC 🏙 🚕 🗽🍎
www.coelholab.com
Columbia SIPA professor studying labor policy, politics of policy design, and political economy. Co-director of Consortium on American Political Economy & Columbia Labor Lab. Former Biden-Harris Department of Labor and Office of Management and Budget.
Postdoc at @BelkaidLab || PhD roots in @iannaconelab 🏳️🌈🏳️⚧️ feminist, LGBTQIA+ soldier, bookworm, 80s flowing in my veins
Senior Scientific Editor @jem.org. Interested in neuroscience, haematology, and lymphatics. Opinions are my own. She/her.
Immunology-focused research in cancer & aging | understanding immune evasion & resilience | improving health outcomes. 🔗 https://genelayinstitute.org/
#Brigham&WomensHospital #MassGeneralHospital @HarvardMed.bsky.social
Immunologist & physician-scientist at Massachusetts General Hospital and Harvard Medical School interested in all things itchy and allergic.
Advancing our understanding of human autoimmunity and transforming patient lives through bold, collaborative, and translational science.
Learn more: www.coltonconsortium.org