Not as much as there should have been.
Do you have something in mind?
Or a question?
10.07.2025 23:59 — 👍 2 🔁 0 💬 1 📌 0
True.
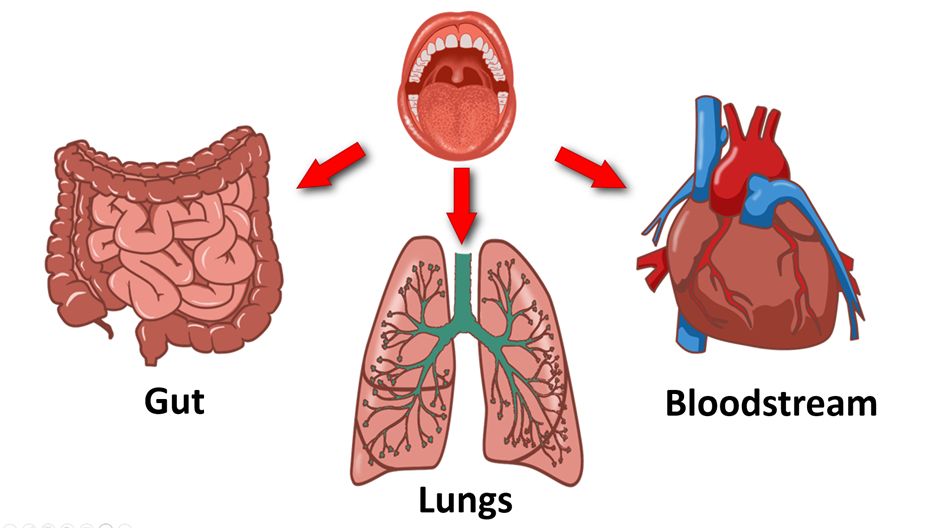
Just saying, to study the gut microbiome without also studying the oral microbiome is like studying the tubes of a trombone without its mouthpiece and wondering where the music comes from.
The oral microbiome determines the gut microbiome.
And the oral microbiome translocates systemically.
04.06.2025 23:45 — 👍 10 🔁 0 💬 1 📌 1
Published today after 2years of work behind the scenes by us at WHN/DELPHI Executive team : Our Global Expert DELPHI Consensus document on Long Covid. 179 Experts from 28 countries around the Globe Participated. Please share. Happy Easter!
link.springer.com/article/10.1...
21.04.2025 00:18 — 👍 159 🔁 74 💬 8 📌 9
Dear #MedBlueSky
Black and white EITHER/OR debates limit us.
Nuanced AND/BOTH debates provide answers.
Let's not oversimplify the human body. It is too complicated to be understood in terms of binary EITHER/OR stances.
The nuance of AND/BOTH is the way forward.
Thanks
18.04.2025 16:38 — 👍 5 🔁 2 💬 0 📌 0
… to ensure correct language is used to describe a disease (not old and potentially misleading language)
And …
To allow challenges to incorrect concepts, to stop them propagating and becoming fixed dogma in the medical literature.
25/25
12.04.2025 23:36 — 👍 29 🔁 1 💬 5 📌 0
I'm now working with likeminded radiologists on an invited review of #COVID imaging for a major radiology journal.
We propose formation of a system by which all medical/scientific specialties collaborate to build understanding when we encounter a new disease …
24/25
12.04.2025 23:36 — 👍 22 🔁 0 💬 1 📌 0
My frustration with the world of medicine (my world) is that we are pathologically unable/unwilling to shift ideas or to see the body holistically.
Our blinkered and siloed approach kills people!
Oral health is the most siloed of all areas of medicine.
23/25
12.04.2025 23:36 — 👍 15 🔁 2 💬 1 📌 0
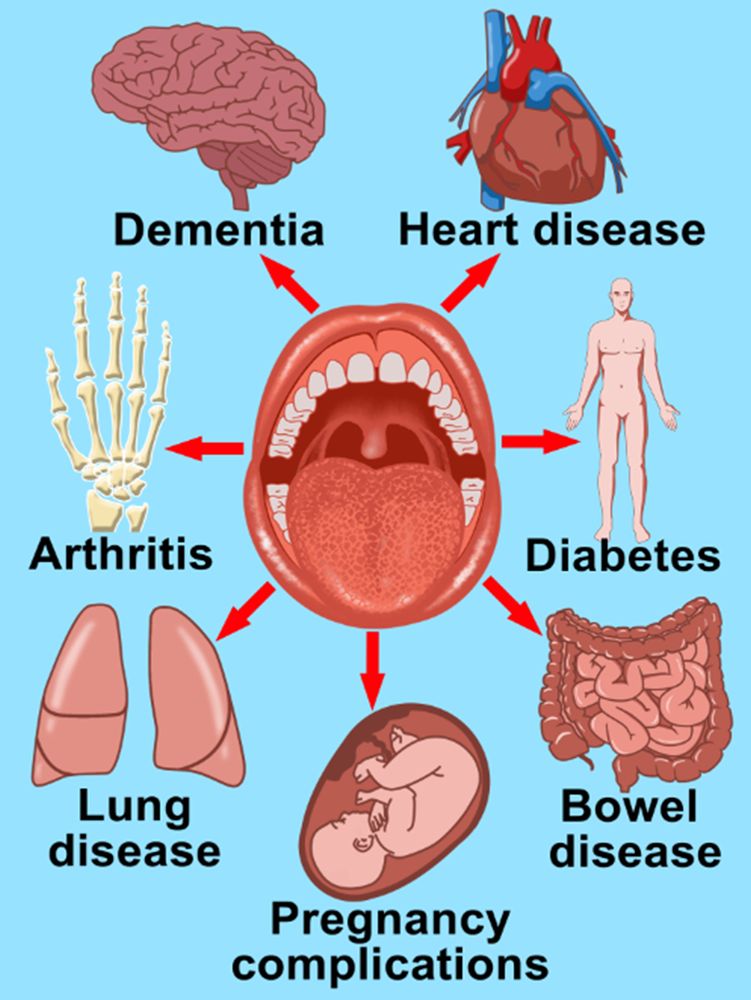
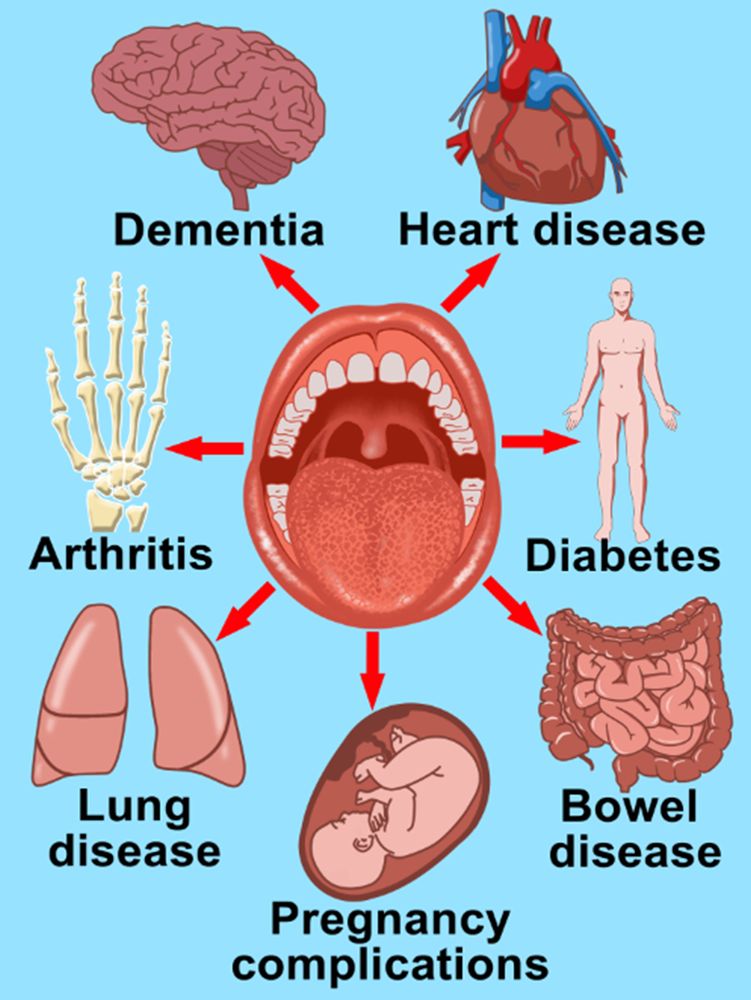
In summary, gum disease bacteria escape the mouth all the time and are directly implicated in biological mechanisms of numerous common diseases of the body including cardiovascular disease, diabetes,
22/25
12.04.2025 23:36 — 👍 15 🔁 3 💬 1 📌 0
YouTube video by Salisbury District Hospital
COVID-19 and the Salisbury Oral Care Pathway
What have I learned from COVID-19? …
That our lack of understanding of the biology of the mouth and the importance of #OralHealth is the biggest missing link in the whole of medicine.
youtu.be/yLhtBZIaAIk
21/25
12.04.2025 23:36 — 👍 20 🔁 5 💬 1 📌 0
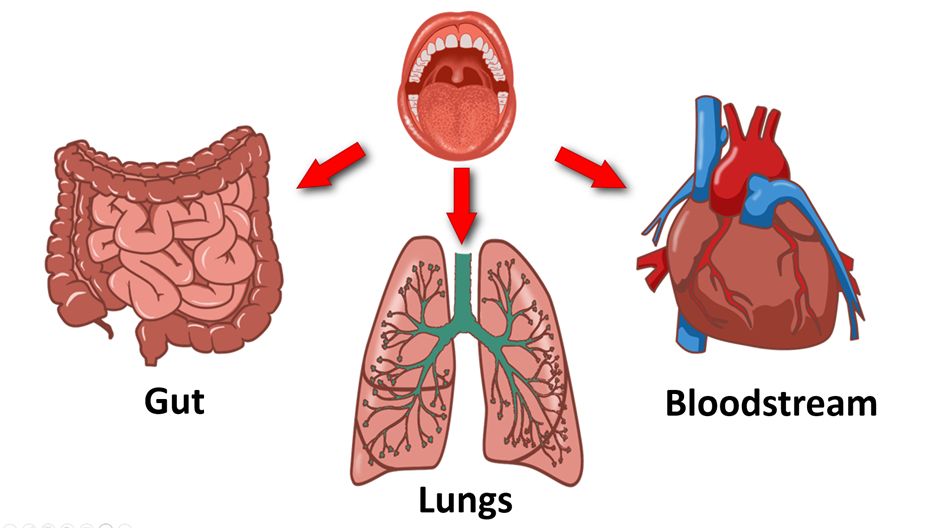
The concept of pathogens escaping the mouth and travelling to the rest of the body is now my major area of interest (writing a book).
20/25
12.04.2025 23:36 — 👍 14 🔁 1 💬 1 📌 0
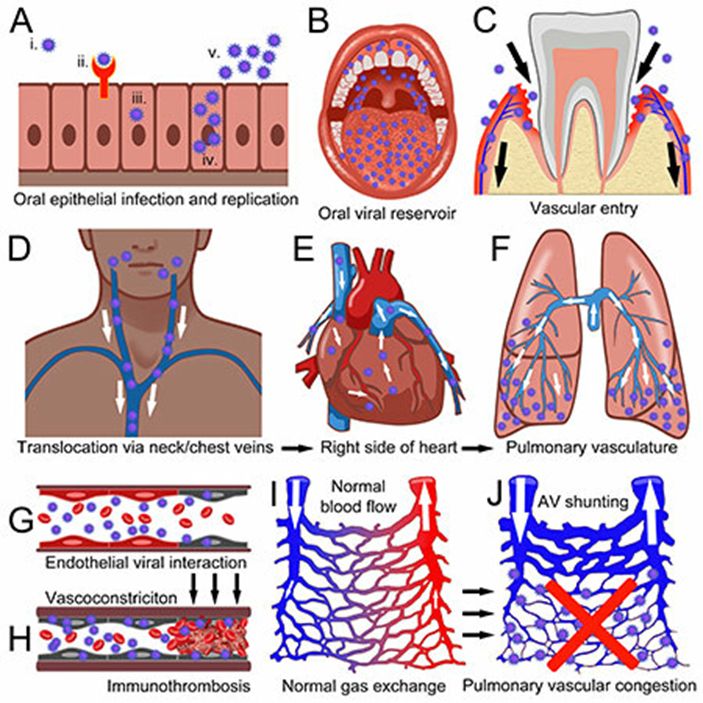
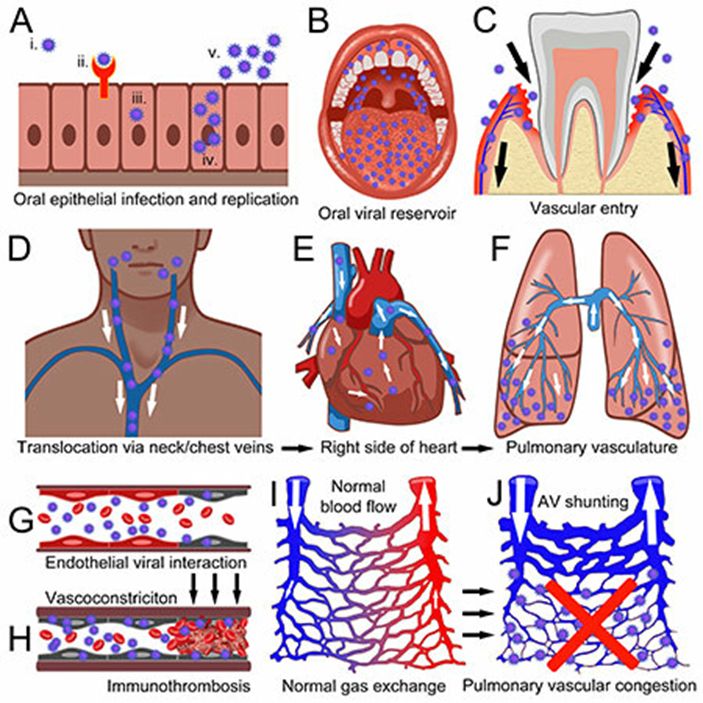
This question led to hypothesizing that the virus is getting to the lungs from the upper respiratory tract (nose and mouth) via the bloodstream.
And this explains why gum disease is a major risk factor for death from COVID-19.
link.springer.com/article/10.1...
19/25
12.04.2025 23:36 — 👍 16 🔁 3 💬 1 📌 0
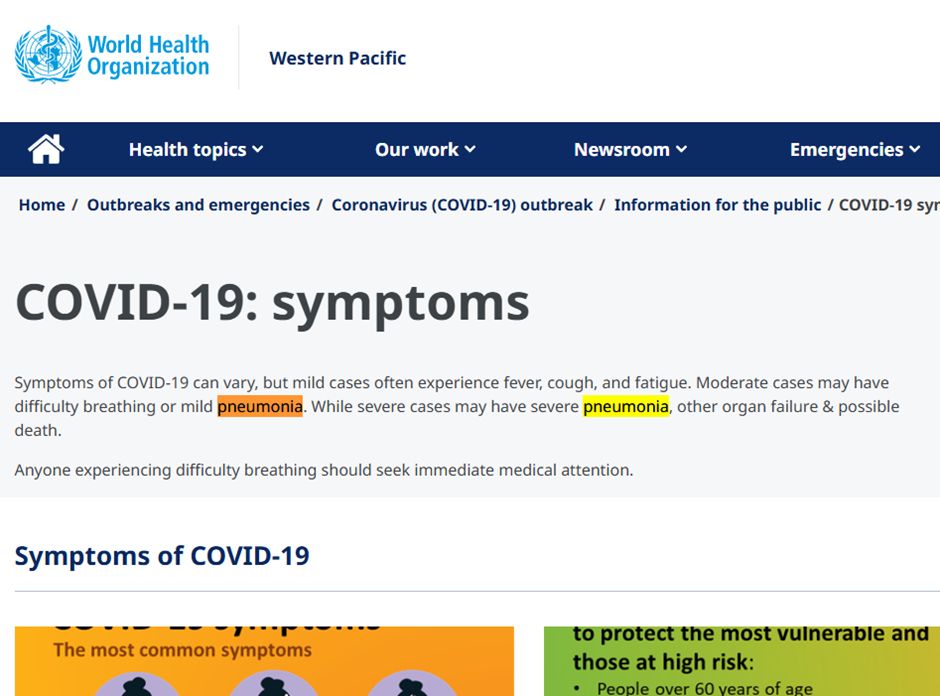
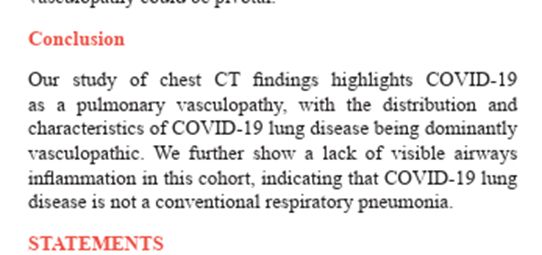
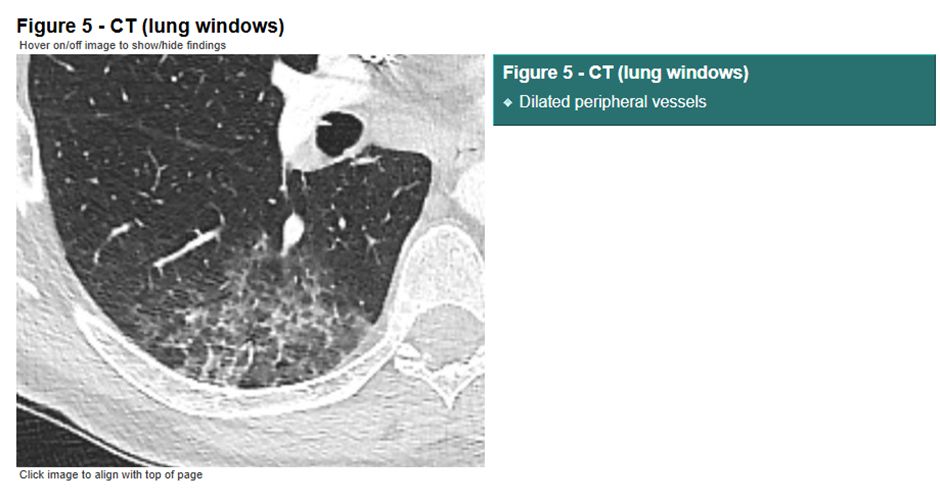
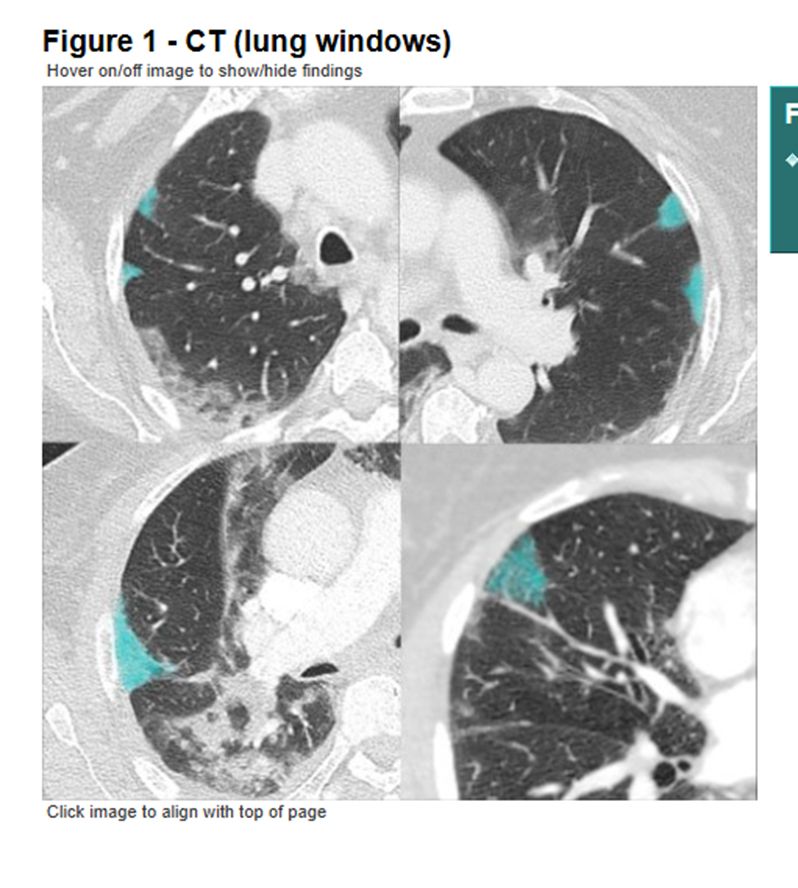
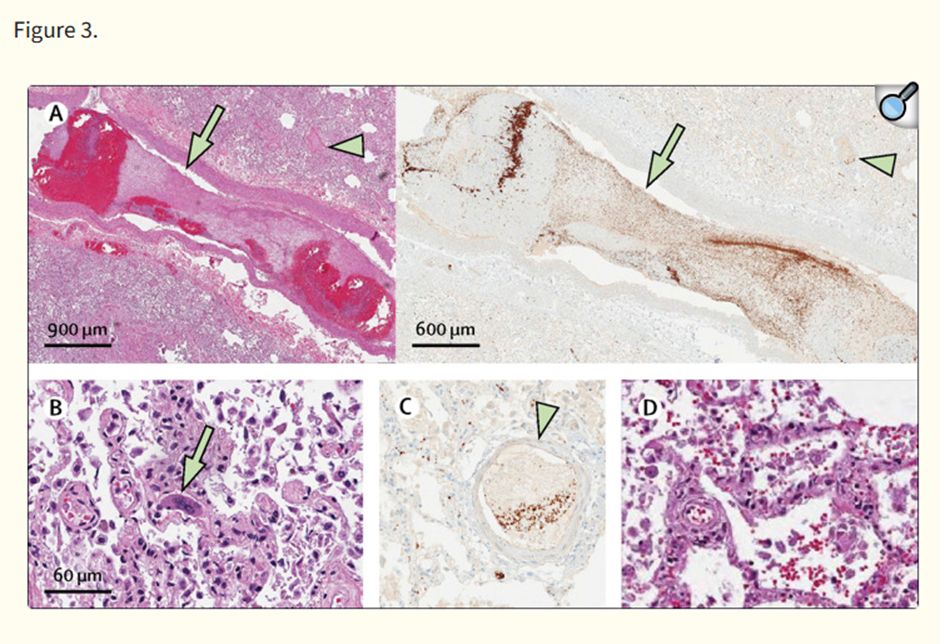
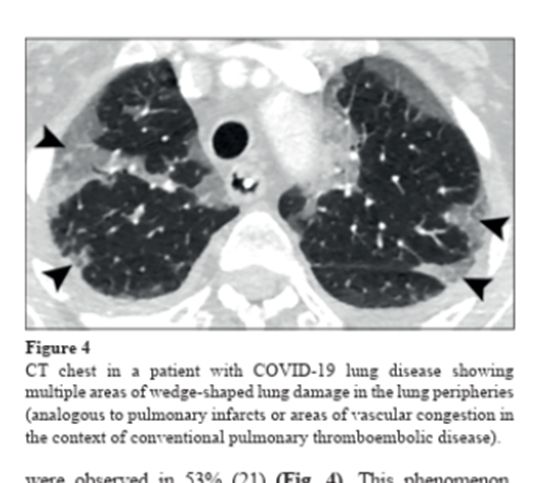
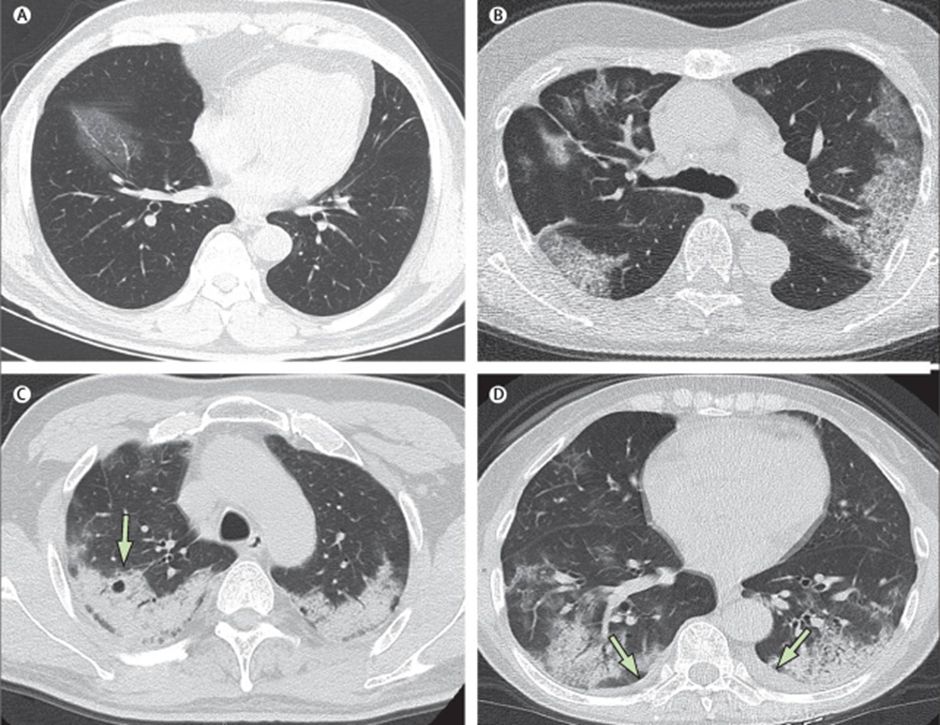
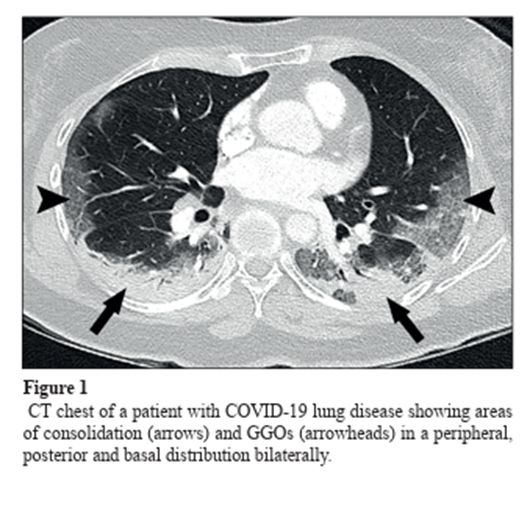
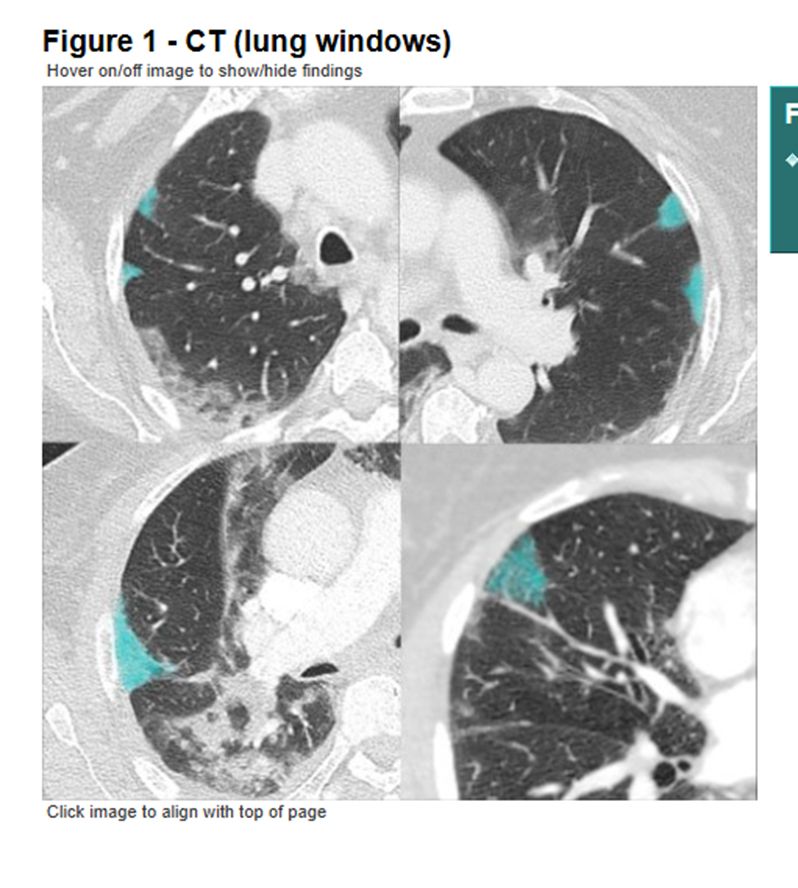
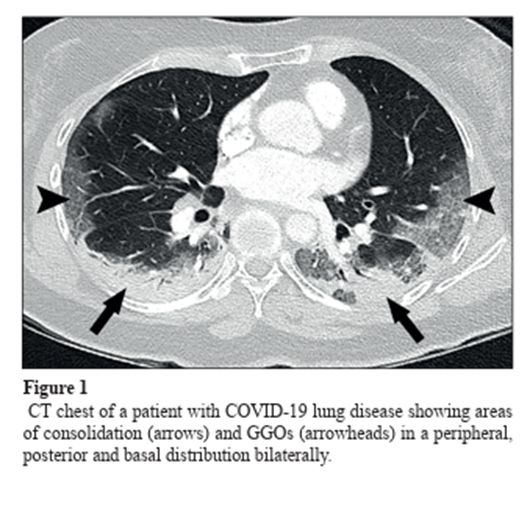
The pattern of lung disease we saw on medical imaging in people with #COVID-19 tells us that the disease is NOT pneumonia, it is a vasculopathy (disease of blood vessels).
This raises another question …
How does this happen?
18/25
12.04.2025 23:36 — 👍 15 🔁 5 💬 1 📌 1
You might think that medical organisations asked – what are we dealing with?
They didn’t!
They assumed it was just like influenza. They kept calling the disease ‘pneumonia’.
This was a fatal error.
17/25
12.04.2025 23:36 — 👍 20 🔁 3 💬 1 📌 0
At the outset of the pandemic, ‘experts’ were called on to advise on population level planning.
This is fine (if you like graphs), but we also need a multidisciplinary approach to attempt to understand the biological mechanisms of the disease we are dealing with.
16/25
12.04.2025 23:36 — 👍 9 🔁 0 💬 1 📌 0
Not ...
What old language can we use to describe this disease?
But ...
What is different?
What is new?
What don't we understand?
And ...
How can we collaborate to build a multidisciplinary understanding of diseases processes?
15/25
12.04.2025 23:36 — 👍 19 🔁 2 💬 1 📌 1
I am posting this story now so that we (humans) can learn some lessons.
When we encounter a new disease, we should all stop and ask ....
What are we dealing with?
Not ...
How is this similar to other diseases we know about?
14/25
12.04.2025 23:36 — 👍 17 🔁 3 💬 1 📌 0
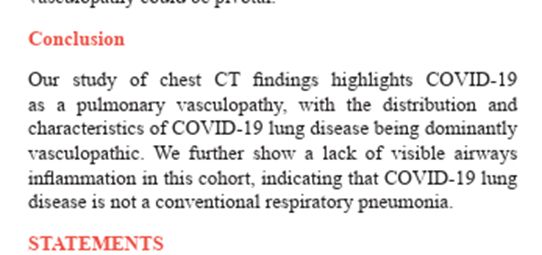
Here is our conclusion …
(Remember, this is 2020 data which could have been published in early 2021)
13/25
12.04.2025 23:36 — 👍 18 🔁 5 💬 1 📌 0
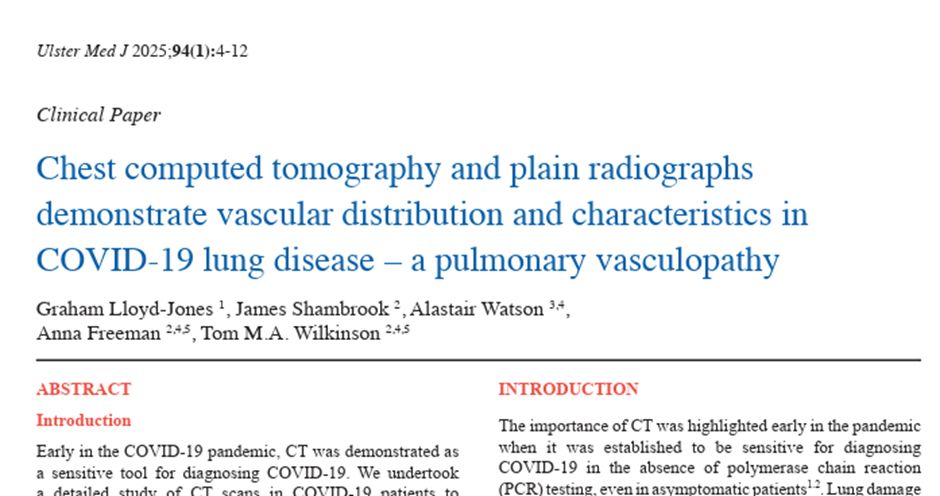
After many attempts to get published we were eventually accepted this month (April 2025!) in an institutional journal.
(Thanks to @UMJBelfast. And thanks especially to my colleague Alastair Watson for not giving up hope of publication.)
bit.ly/4j6fIpx
12/25
12.04.2025 23:36 — 👍 19 🔁 2 💬 1 📌 0
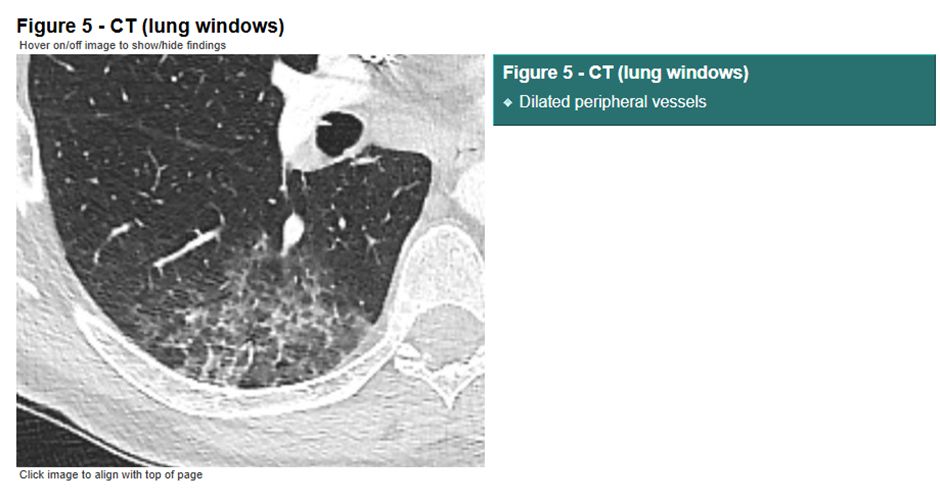
The airways of the lungs were NORMAL!
Unlike influenza, there was no inflammation in the lung airways in people with #COVID-19.
The blood vessels were damaged.
And yet the world of medicine carried on treating it as if it were flu.
11/25
12.04.2025 23:36 — 👍 22 🔁 3 💬 2 📌 0
This led to an invitation to join the REACT COVID-19 research group based in Southampton, UK. I was initially the sole radiologist on the project.
People from across the world sent me examples of COVID-19 cases. I looked at thousands of images. The same pattern was repeated …
10/25
12.04.2025 23:36 — 👍 11 🔁 1 💬 1 📌 0
YouTube video by Radiology Masterclass
COVID-19 Lung Disease: A Pulmonary Vasculopathy
In November 2020 I was invited to speak at the @BritSocHaem annual conference.
The talk highlights that #COVID-19 is NOT a pneumonia. It is a pulmonary vasculopathy (disease of the lung blood vessels).
youtu.be/2jROYLwUK20
9/25
12.04.2025 23:36 — 👍 12 🔁 4 💬 1 📌 0
So I published informally as a blog on the Radiology Masterclass website and shared my ideas widely.
bit.ly/3E6PX9D
8/25
12.04.2025 23:36 — 👍 10 🔁 1 💬 1 📌 0
In June 2020 I wrote to a UK radiology journal to raise the alert.
The title of my letter was – ‘Acute COVID-19 lung disease: A pulmonary vasculopathy not a pneumonia’
I was told it would be too ‘time-consuming’ to be put forward for publication.
7/25
12.04.2025 23:36 — 👍 11 🔁 2 💬 1 📌 0
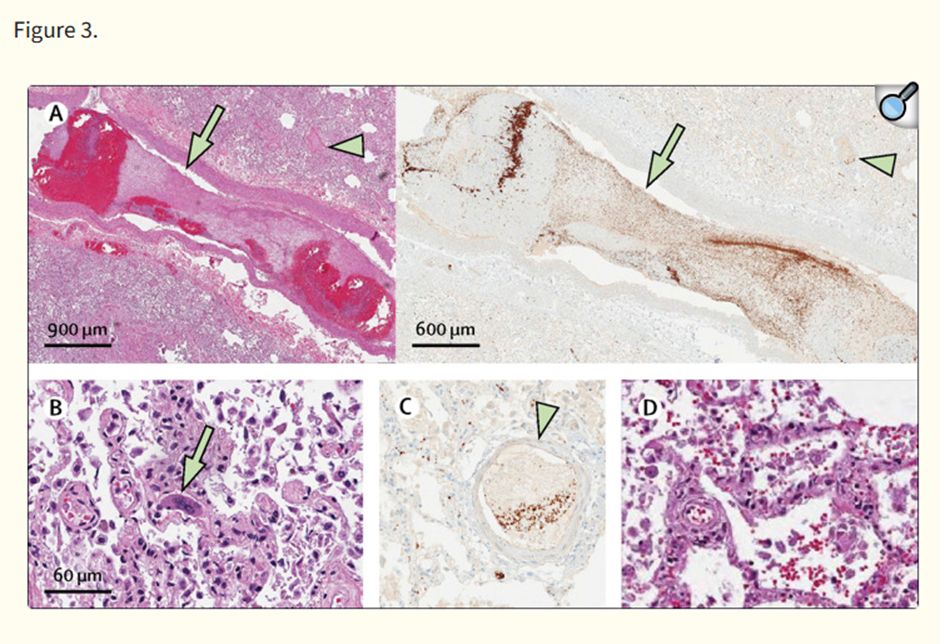
Soon the autopsy papers showed that clotting in the lungs was occurring in the capillaries (the smallest blood vessels). This means that we would not be able to detect clotting in the lungs using standard imaging techniques.
bit.ly/3XSg8aM
6/25
12.04.2025 23:36 — 👍 11 🔁 2 💬 1 📌 0
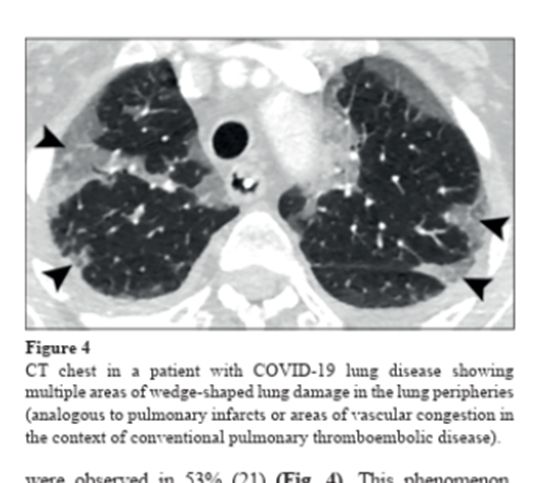
I wanted to know WHY #COVID-19 caused this weird ‘pneumonia’.
The areas of lung damage looked like what we see when someone has blood clots in the lungs.
bit.ly/4j6fIpx
5/25
12.04.2025 23:36 — 👍 9 🔁 2 💬 2 📌 0
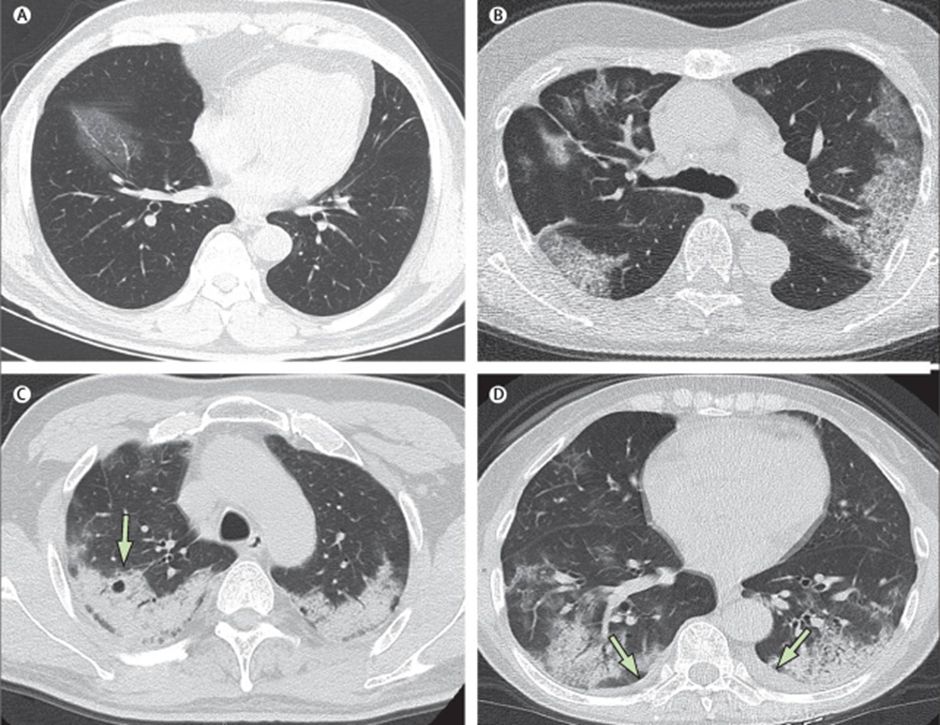
The early papers from China showed distinct patterns of lung damage on CT scans which helped to make the diagnosis, but this was not the main question I had.
bit.ly/43PTfZi
4/25
12.04.2025 23:36 — 👍 9 🔁 1 💬 1 📌 0

COVID-19 Image Gallery
In early 2020 I had an obvious job to do – teach doctors to make the diagnosis of COVID-19 on a chest X-ray or CT scan.
Making the diagnosis is easy because COVID-19 causes a lung disease which is totally unlike other ‘pneumonias’.
bit.ly/3XSvMmr
3/25
12.04.2025 23:36 — 👍 10 🔁 1 💬 1 📌 0
Firstly, who am I?
I am an educator in medical imaging, best known for founding Radiology Masterclass, a leading online resource for radiology education.
www.radiologymasterclass.co.uk
2/25
12.04.2025 23:36 — 👍 8 🔁 1 💬 1 📌 0
If in Dec 2020 you had told me it would take until April 2021 to get my #COVID research published, I’d have been disappointed.
It has now been published (April 2025), 4 years later.
bit.ly/4j6fIpx
👇
Here's my epic COVID-19 failure story …
Long thread 1/25
12.04.2025 23:36 — 👍 71 🔁 32 💬 6 📌 8
Association of British Science Writers advocates and provides professional training, development and networking for journalists and writers covering STEM.
Freelance Science Broadcaster🎙️| Presenter of CrowdScience on The BBC World Service | Views are my own (unless determinism has other ideas)
Links to website and other socials ⬇️
https://linktr.ee/carolinesteel
Chair of British Dental Association
Lawyer, Filmmaker, Big Issue top 100 Changemaker 2024, CEO CAMPAIGN FOR SOCIAL JUSTICE https://www.cfsj.co.uk/
Dentist, dad, husband and Chair @theBDA.bsky.social General Dental Practice Committee
Dr. phil.; former professor; #Sozialpädagogik #Demokratiebildung #KinderundJugendarbeit #socialwork #Antifaschist #fcsp 🤎🤍❤️ Check: emptystands.me
Homepage: https://www.bildung.uni-siegen.de/mitarbeiter/fritz
Comedian. Travel Writer. Fainéant.
Bookings- lesley@aitkenalexander.co.uk
Radionuclide Radiologist | Head of Severn School of Radiology
President of the Royal College of Radiologists, Consultant Cardiothoracic Radiologist in Southampton. All views are my own
Kindness, Empathy, Love always.
Covid damages your health.🦠
Bird Flu (H5N1) maybe soon too
N95😷 to keep each other safe
My List - Covid Info/Science
I have friends on here who need us to use the alt text feature on images. Try and remember to 🙏🏻
Academic dentist.
Work = Restorative dentistry & diabetes.
Life = family, sports, nature, travel.
Storyteller.
I write.
I research.
I photograph.
Archaeologist of hidden stories.
Witness.
Orchids.
Available for commissions.
Paypal.me/MarjorieHMorgan
ko-fi.com/Marjorie
Bylines: Art UK, gal-dem, Are We Europe, Corridor8, The Fourdrinier
UK based charity advocating for those impacted by #LongCovid
Recognition - Research - Rehabilitation
www.longcovidsos.org
info@longcovidsos.org
Charity reg no 1199120
GP, medical educator, writer (BMJ columnist, Dr Helen in 'Take a Break') Independent SAGE, BMA Council.
Special care dentist, interested in improving oral health for people with disabilities.
Labour MP for Ilford North. Secretary of State for Health & Social Care.
Social Epidemiologist, Medical Sociologist, Quantitative Methodoloigst | Associate Professor Sociology @uoregon |
Views are my own | Repost =/= endorse |
Intersectional MAIHDA, health inequities researcher
Professor, University of California, Riverside School of Public Policy. Faculty Director, Science to Policy (S2P). Public health scientist & sociologist keen on population health & community issues. Sometimes in the news, often for troubling topics. 🇺🇸 🇨🇦
Director @ Campus PR | Research Communicator | Science Writer | Dysgu siarad Cymraeg | Previously OxUni, MRC and British Science Association. www.campuspr.co.uk
#scicomm #stempr 🌈🖖