
Confused about steroids in the ICU? This week on the podcast, we talk to David Janz about who needs them, which ones to use, and which dose. icuscenarios.com/lightning-ro...
26.11.2025 13:17 — 👍 2 🔁 0 💬 1 📌 0@criticalcarenotes.bsky.social
Critical Care Nurse Practitioner. FCCM. One half of the icuscenarios.com podcast and the icu101.com team. criticalcarenotes.com

Confused about steroids in the ICU? This week on the podcast, we talk to David Janz about who needs them, which ones to use, and which dose. icuscenarios.com/lightning-ro...
26.11.2025 13:17 — 👍 2 🔁 0 💬 1 📌 0
DOPES Mnemonic: structured approach to deal with hypoxia in the ventilated patient
Displacement, Obstruction, Patient factors (ie PE, PTX), Equipment Issues, Stacked Breaths.
Address all of these factors in parallel
youtube.com/shorts/rwumW...
#EMIMCC
I have a long standing belief that procrastination often pays off. You just have to known WHEN to procrastinate.
30.10.2025 11:06 — 👍 2 🔁 0 💬 1 📌 0Remembering the most likely mediator of reduced mortality in the original EGDT therapy was the presence of the CI in the intervention arm, the regular attendance of an interested and informed clinician (and skilled ICU nurse) likely has a bigger impact than any single drug or intervention.
29.10.2025 16:08 — 👍 30 🔁 9 💬 4 📌 1 22.10.2025 20:29 — 👍 2 🔁 1 💬 0 📌 0
22.10.2025 20:29 — 👍 2 🔁 1 💬 0 📌 0

Just updated the IBCC chapter on cholecystitis & cholangitis.
These patients are often initially triaged to the ICU.
Understanding these diseases can help us direct patients to interventions they need.
Let’s talk about four pearls 😁
chapter: emcrit.org/ibcc/biliary... #EMIMCC
A man in his 50s seeks the ED for the umpteenth time since his abdo pain started a few years ago. He says that it’s his gallbladder, surgery has been denied because of diffuse pain and normal blood tests. Today CRP 9, Leukocytes 11. #POCUS He got his operation the next day. #EMIMCC
09.10.2025 09:45 — 👍 12 🔁 3 💬 1 📌 0I do this pretty regularly
24.08.2025 10:34 — 👍 1 🔁 0 💬 0 📌 0
Point-of-care ultrasound is being used by an increasing number of nurse practitioners, but its utility is not limited to the ICU, nor even to Acute Care.
journals.lww.com/jaanp/abstra...

rapidly pushing IV calcium may cause:
😦 vasodilation, bradycardia, hypotension
😦 nausea/vomiting, flushing
if patients are conscious, this can make them feel horrible
if the patient is obtunded & not intubated, emesis can be a big problem
whenever possible, give IV Ca slowly #EMIMCC
The other thing to remember is that patients in HFNC typically benefit more from “flow” than FiO2. So wean the FiO2 before the flow.
01.08.2025 22:25 — 👍 2 🔁 0 💬 0 📌 0And remember, ST is often compensatory. Don’t slow it down blindly.
22.07.2025 09:34 — 👍 1 🔁 0 💬 0 📌 0“But WHY did they fail?” All too often I get, “they failed SBT” from someone who also wasn’t there, and that’s that. Do it again and see for yourself. Often you can get them off the vent after all.
22.07.2025 09:33 — 👍 2 🔁 0 💬 0 📌 0Big news for lung ultrasound #POCUS
21.07.2025 12:14 — 👍 2 🔁 1 💬 0 📌 0I sadly see this not rarely. Especially with overworked interns. They run out of time and rather than admit this, and risk being perceived as failing, they lie. And they ALWAYS get caught.
04.07.2025 23:40 — 👍 0 🔁 0 💬 0 📌 0I’ll add to this, communicate when you want to be called. Don’t just start NE with a MAP goal>65, add, “call me if you get to X.” This prevents you getting busy and checking back to find that they’re almost maxed.
02.07.2025 20:51 — 👍 1 🔁 0 💬 0 📌 0
Occult VF in Cardiac Arrest: 5.3% of patients with cardiac arrest showed VF on echo but ECG w/ PEA/asystole
Study does not show improved outcomes but not powered to do so
Strong argument for intra-arrest echo as it can dramatically change management
#EMIMCC
Advice for New Trainees #2: Listen to your nurses
Don’t mistake your short time as a doctor as equivalent clinically to their years and decades of experience
If a nurse asks you to reevaluate a patient, GO TO THE BEDSIDE AND RE-EVALUTE THE PATIENT, EVERY TIME.
youtube.com/shorts/c0o5F...
#EMIMCC
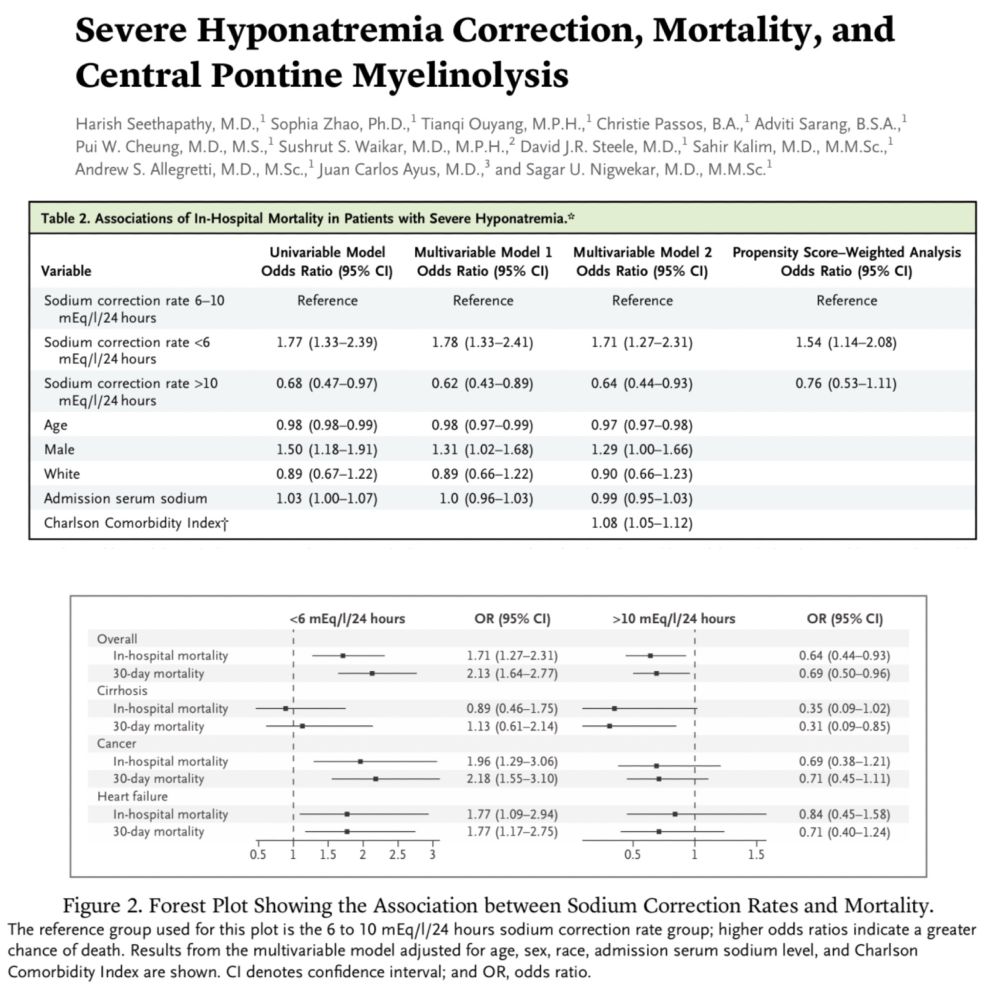
Might we be correcting hyponatremia too slowly? May our patients be suffering because we're too fearful of the risk of central pontine myelinolysis? Here's data that may challenge our regular approach. Hat tip to the authors.
eddyjoemd.com/foamed
Interesting. Had never thought of this before. How many other things in medicine to we get wrong because if assumptions?
27.06.2025 11:45 — 👍 1 🔁 0 💬 0 📌 0
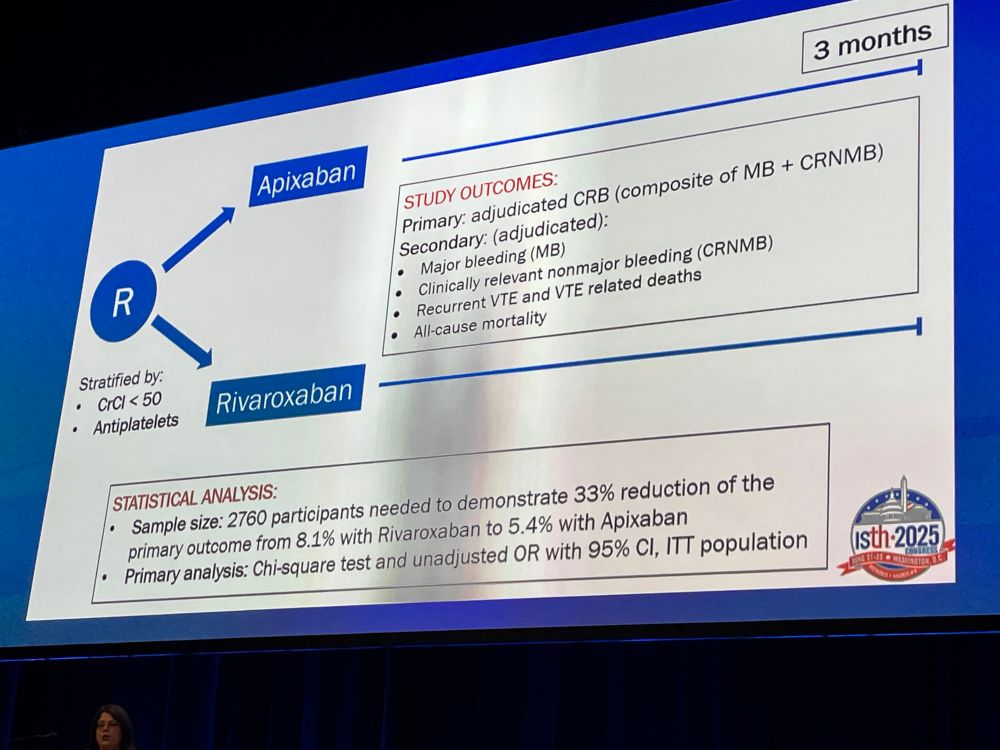
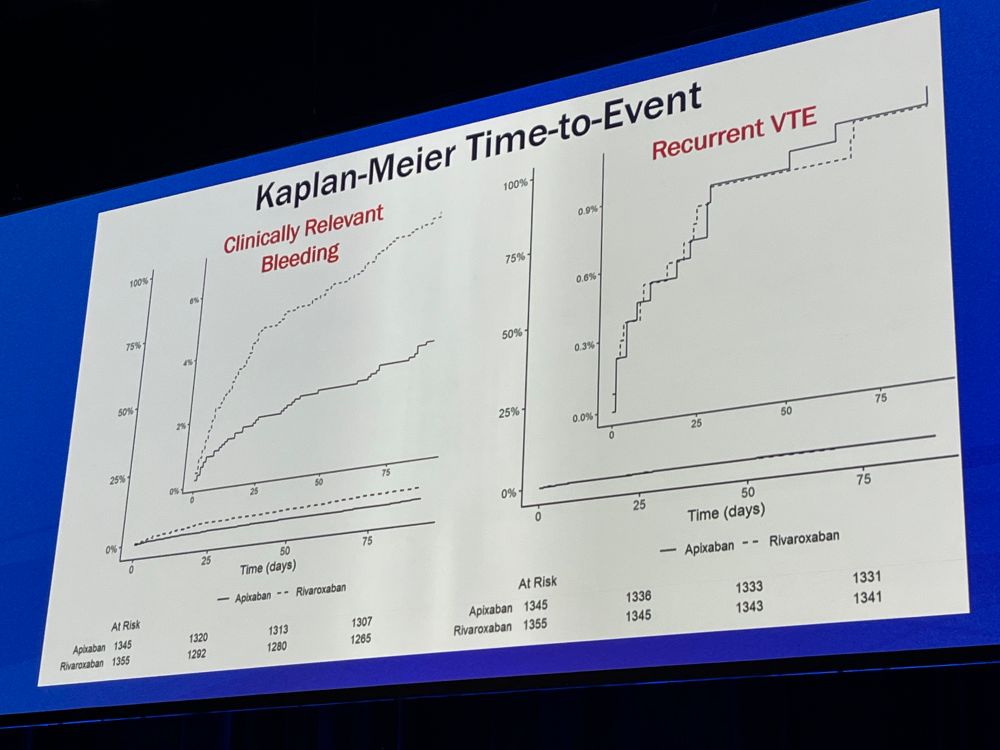
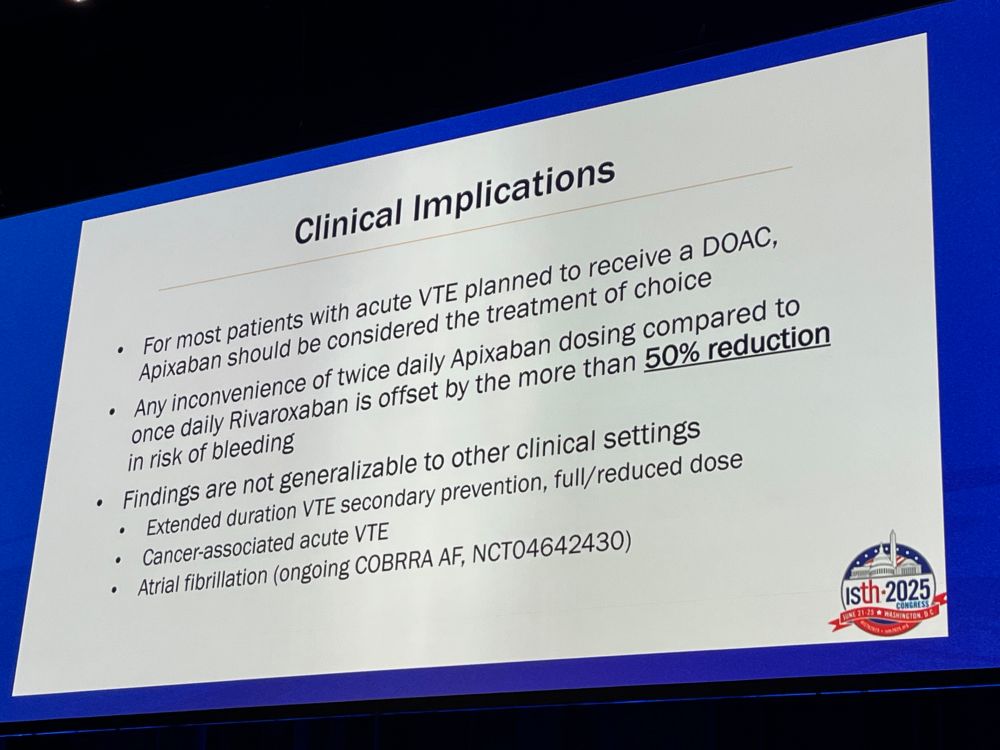
This is what we were waiting for. A direct comparison between apixaban and rivaroxaban for the treatment of acute VTE. Apixaban reduces bleeding risk in the first 3 months by >50%!
Practice changing investigator-initiated RCT.
#ISTH2025
Recently had @ebtapper.bsky.social on the Critical Care Scenarios podcast talking GI and this topic came up.
icuscenarios.com/lightning-ro...
Totally agree regarding docusate. I start bowel regimen (typically senna) on admission. Like pain, much easier to get ahead of than to fix when out of control. Escalate as needed. BM at least every 3 days.
18.06.2025 11:32 — 👍 1 🔁 0 💬 1 📌 0Not anesthesia but all my attendings are. We typically reverse prior to extubation in cases like you mention.
18.06.2025 11:29 — 👍 1 🔁 0 💬 0 📌 0New lesson in the POCUS course: Abdominal ultrasound!
#medsky #emimcc #POCUS
Mottling is one of this signs that gets me real worried.
16.06.2025 12:24 — 👍 4 🔁 2 💬 0 📌 0
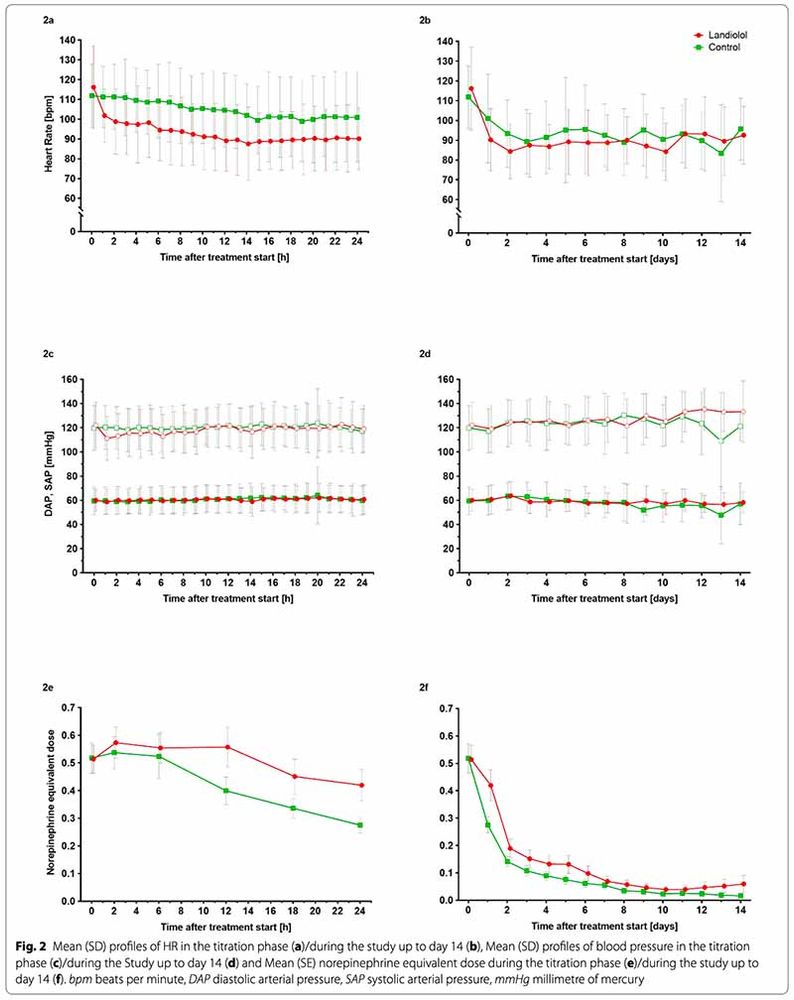
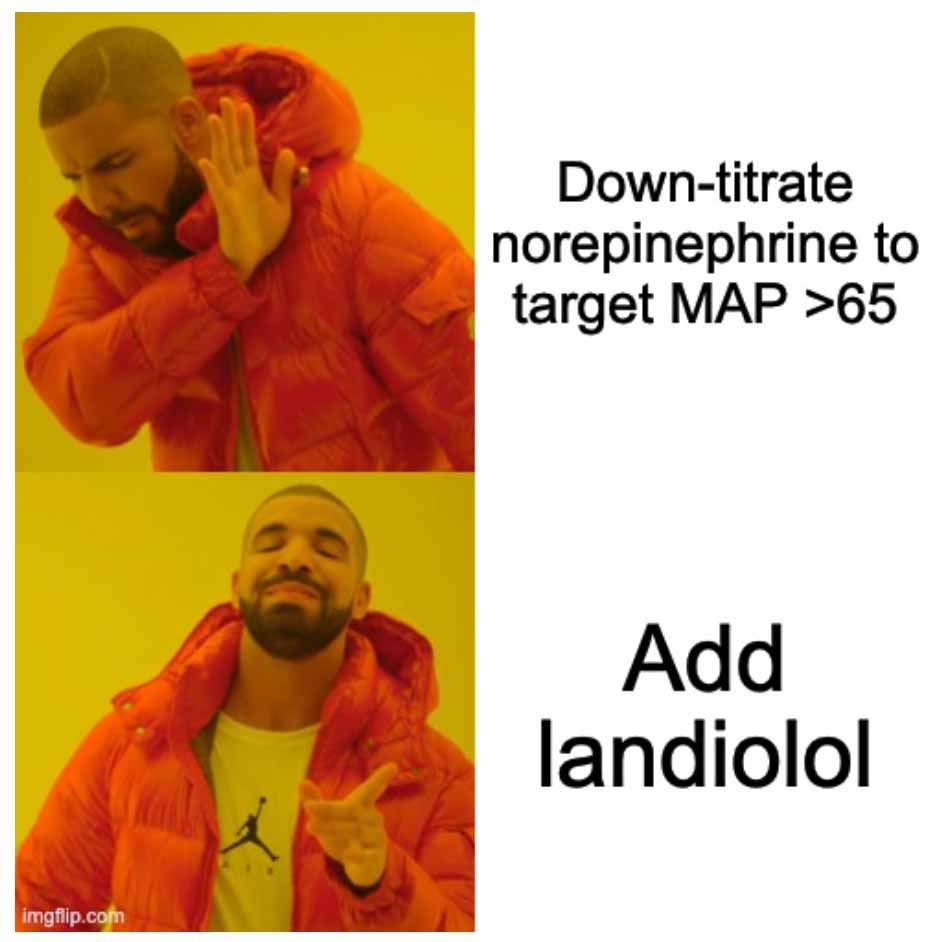
beta-blocker in sepsis trials continue to mystify me
you have patients on reasonable doses of pressor (0.5 mcg/kg/min norepi equivalent) with an average MAP ~80 (mean diastolic BP ~60!)
you're worried about catecholamine toxicity
instead of reducing the pressors you add a beta-blocker😳 #EMIMCC
Don’t be distracted by the obvious pleural yuck…
16.06.2025 12:17 — 👍 0 🔁 0 💬 0 📌 0My students know well of my disdain for the d-diner…
16.06.2025 12:16 — 👍 0 🔁 0 💬 0 📌 0About all it’s good for.
16.06.2025 12:15 — 👍 2 🔁 0 💬 0 📌 0