Development of a Machine Learning–Based Predictive Model for Postoperative Delirium in Older Adult Intensive Care Unit Patients: Retrospective Study
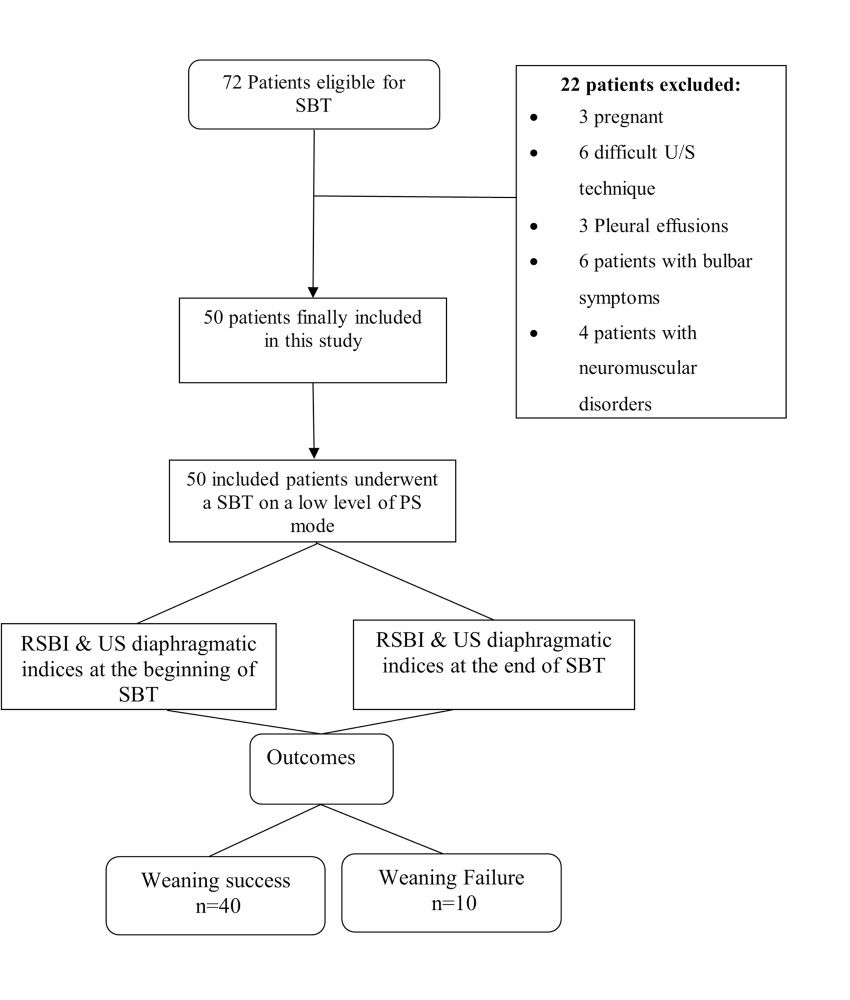
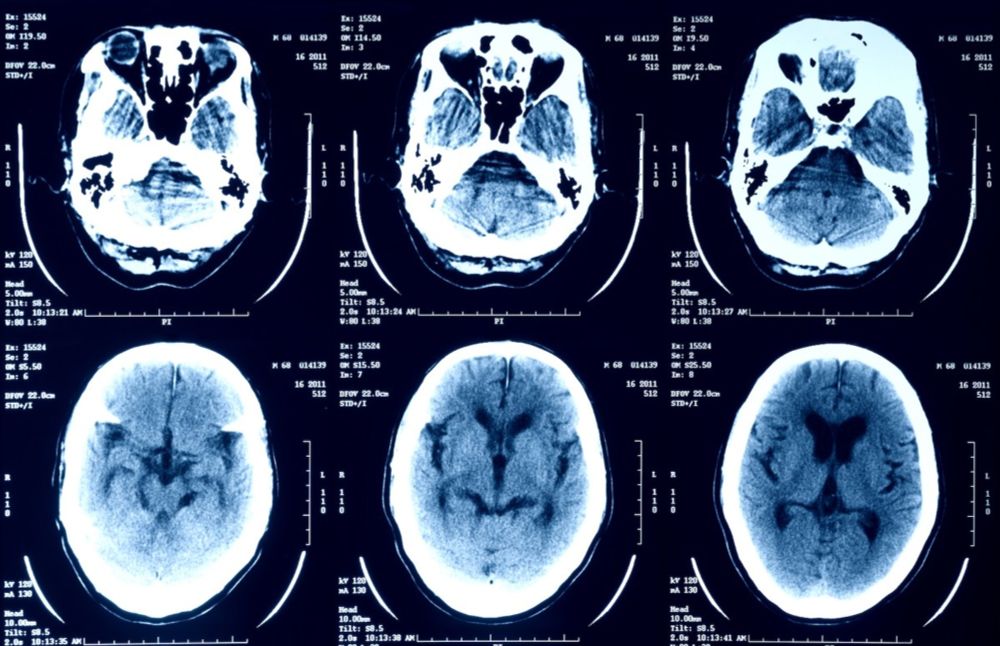
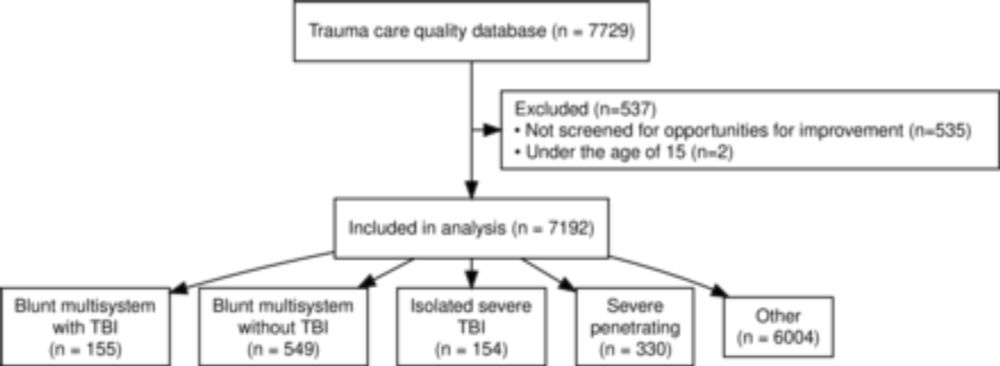
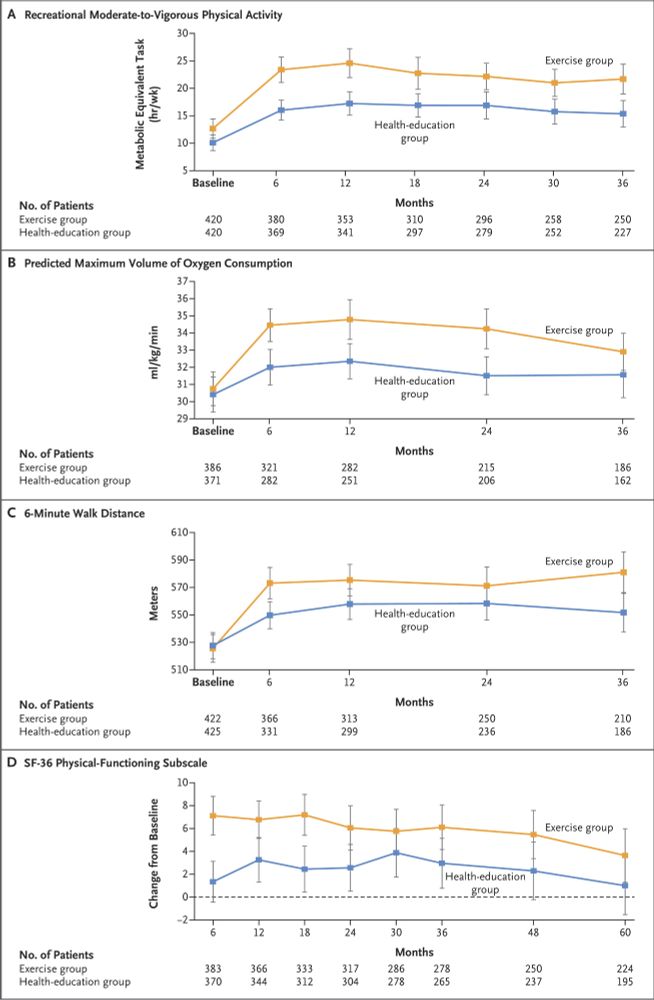
Background: Delirium is a prevalent phenomenon among patients admitted to the geriatric intensive care unit (ICU) and can adversely impact prognosis and augment the risk of complications. Objective: We aimed to construct and validate a predictive model for postoperative delirium state in older ICU patients, providing timely and effective early identification of high-risk individuals and assisting clinicians in decision-making. Methods: The data from patients admitted to the ICU for over 24 hours were extracted from the Medical Information Marketplace for Intensive Care IV (MIMIC-IV) database and the eICU Collaborative Research Database (eICU-CRD). The MIMIC-IV data were split (7:3) into training and internal validation sets, while the eICU-CRD data served as an external validation set. Delirium predictions were conducted for the subsequent prediction windows (12 h, 24 h, 48 h, and whole stay time) using data from the first 24 hours post admission. The corresponding feature variables were subjected to Boruta feature selection, and the prediction models were constructed using logistic regression, support vector classifier, random forest classifier, and extreme gradient boosting (XGB). Subsequently, model performance was evaluated using areas under the receiver operating characteristic curves (AUCs), Brier scores, and decision curve analysis, and external validation. Results: The MIMIC-IV and eICU-CRD datasets comprised 6129 and 709 patients, respectively, who were included in the analysis. Fifty-four features were selected to construct the predictive model. Regarding internal validation, the XGB model demonstrated the most effective prediction of delirium across different prediction windows. The AUCs for the 4 prediction windows (12 h, 24 h, 48 h, and whole stay time) were 0.848 (95% CI 0.826-0.869), 0.852 (95% CI 0.831-0.872), 0.851 (95% CI 0.831-0.871), and 0.844 (95% CI 0.823-0.863), respectively, and those of the external validation set were 0.777 (95% CI 0.726-0.825), 0.761 (95% CI 0.710-0.808), 0.753 (95% CI 0.704-0.798), and 0.737 (95% CI 0.695-0.777), respectively. Furthermore, the XGB model demonstrated the most accurate calibration across all prediction windows, with values of 0.129, 0.136, 0.144, and 0.148, respectively. Additionally, decision curve analysis revealed that the XGB model outperformed the other models in terms of net gain for the majority of threshold probability values. The 6 most significant predictive features identified were the first day’s delirium assessment results, type of first care unit, minimum Glasgow Coma Scale (GCS) score, Acute Physiology Score III, acetaminophen, and nonsteroidal anti-inflammatory drugs. Conclusions: The high-performance XGB model for predicting postoperative delirium state in older adult ICU patients has been successfully developed and validated. The model predicts the delirium state at 12 h, 24 h, 48 h, and whole stay time after the first day of hospitalization within the ICU. This enables physicians to identify high-risk patients early, thus facilitating the optimization of personalized management strategies and care plans.
Development of a Machine Learning–Based Predictive Model for Postoperative Delirium in Older Adult Intensive Care Unit Patients: Retrospective Study