Image references:
1. DOI: 10.1586/17474086.2014.954541
2. DOI: 10.1016/j.amjmed.2020.03.005
3. my.clevelandclinic.org/health/disea...
4. my.clevelandclinic.org/health/diagn...
5. www.irhythmtech.com/us/en
@isaaclamb01.bsky.social
PGY-4 neurology resident. Interested in clinical neurology, medical education, history, and nerd stuff.
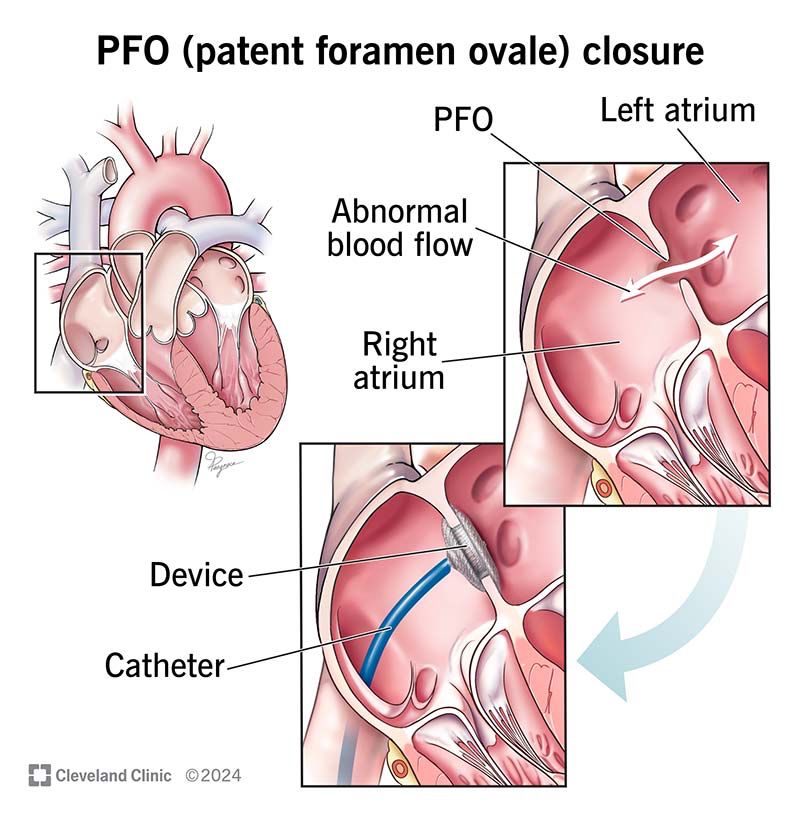
Image references:
1. DOI: 10.1586/17474086.2014.954541
2. DOI: 10.1016/j.amjmed.2020.03.005
3. my.clevelandclinic.org/health/disea...
4. my.clevelandclinic.org/health/diagn...
5. www.irhythmtech.com/us/en
SUMMARY:
- Imaging: strokes in multiple territories
- Workup: TTE with bubble, cardiac monitoring, +/- TEE
- Management
> Afib: AC (DOAC preferred) vs LAA occlusion
> PFO: refer for closure if high risk
> Ventricular thrombus: warfarin
I’ll point out that there are other central embolic strokes that we didn’t talk about here because I’m planning to discuss them later:
- ESUS (cryptogenic)
- Septic embolism / endocarditis
- Arterial hypercoagulability
Stay tuned for a future thread on these!
Ventricular thrombi and valvular afib have not been as well studied. Current AHA guidelines recommend warfarin over DOACs but this is mostly due to a paucity of evidence.
12.07.2025 20:52 — 👍 0 🔁 0 💬 1 📌 0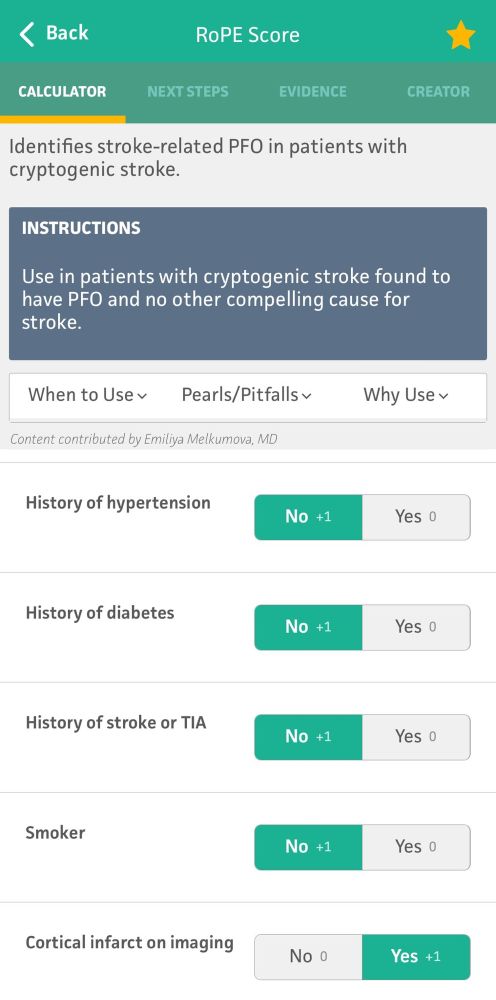
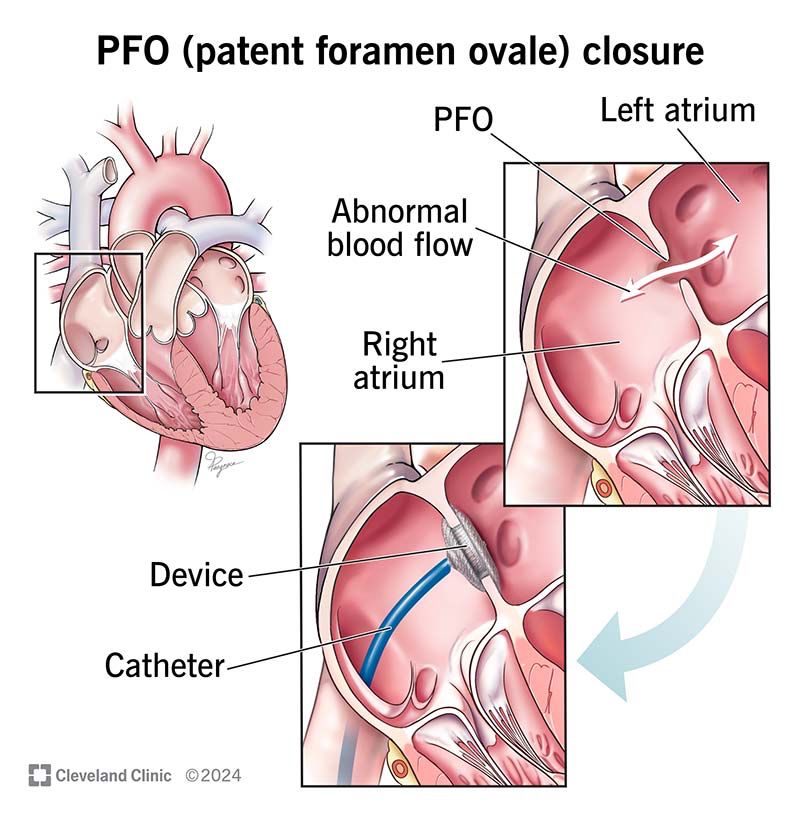
Should you close a PFO?
Not necessarily. About 20% of the population has a PFO. Most strokes, even in patients with a PFO, were probably from something else.
The decision to close one is based off of size, imaging, patient age and risk, and scoring tools (eg RoPE score).
The decision to cardiovert is another important one. Options include both chemical and electrical cardioversion and generally requires either short term anticoagulation or a TEE to exclude thrombus. Generally, this decision is up to the cardiologist.
12.07.2025 20:52 — 👍 0 🔁 0 💬 1 📌 0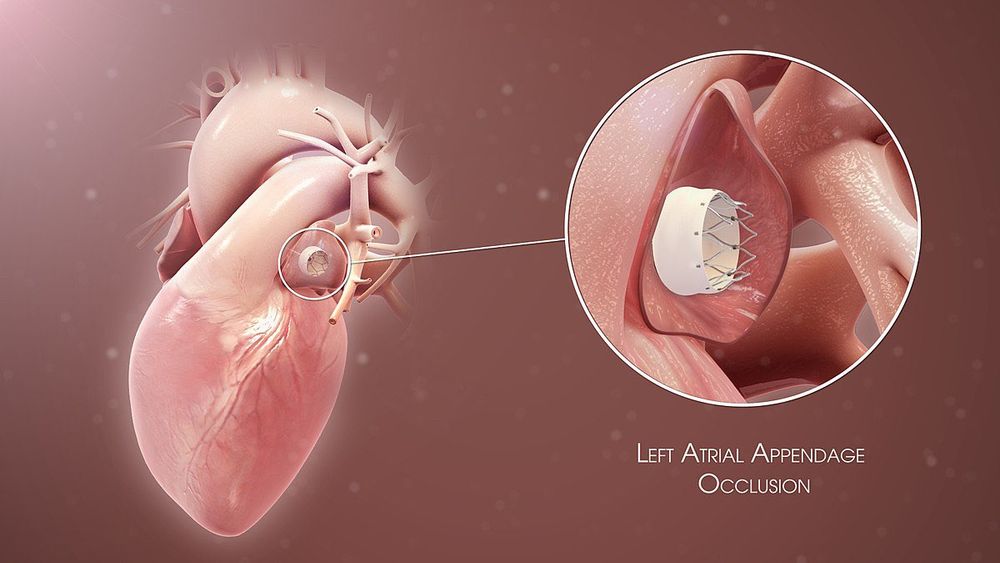
TREATMENT
Most afib patients require chronic anticoagulation, and this is doubly true for stroke patients. Studies have shown superiority in DOACs (eg apixaban) over warfarin. If patients have contraindications to chronic AC, a LAA occlusive device gets almost the same benefit.
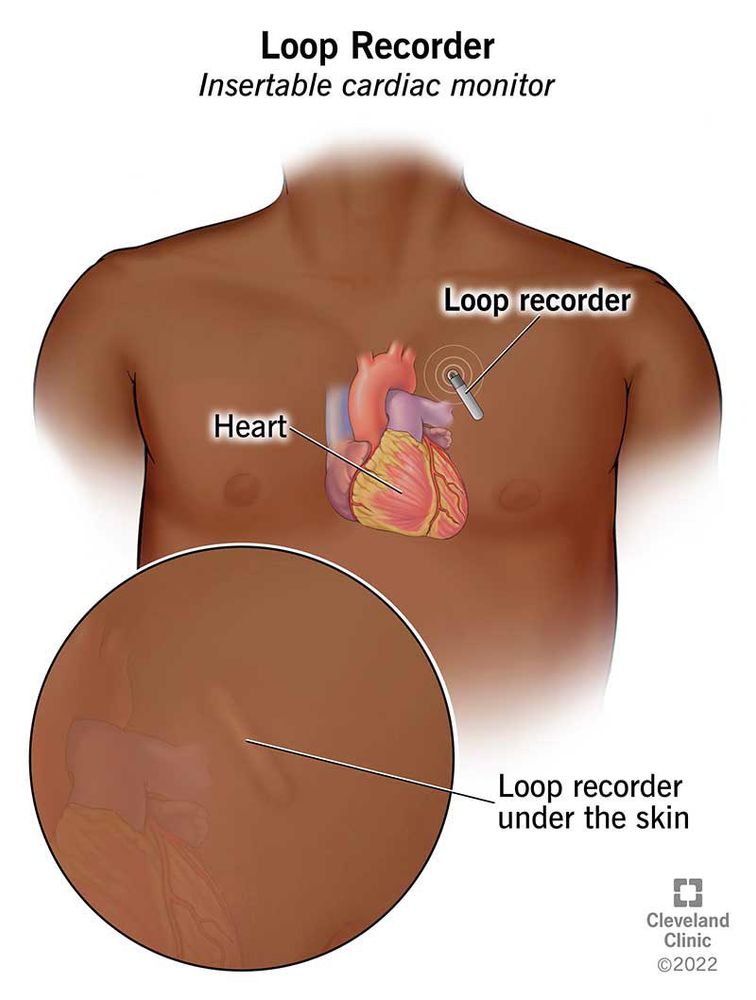

While we monitor all stroke patients while inpatient, statistically many cases of afib are paroxysmal and will be missed. We use a variety of ambulatory cardiac monitoring devices on discharge to improve sensitivity.
12.07.2025 20:52 — 👍 0 🔁 0 💬 1 📌 0Afib can be detected as easily as via a simple EKG, but interpretation is tricky. What if they were only in afib for a few minutes secondary to heart strain from the stroke? Or what if they are back in NSR?
12.07.2025 20:52 — 👍 0 🔁 0 💬 1 📌 0Emerging diagnostic modalities include cardiac CT, which has shown particular value for identifying ventricular thrombus and doesn’t come with the procedural risks of TEE.
12.07.2025 20:52 — 👍 0 🔁 0 💬 1 📌 0If we have a high suspicion for either LAA thrombus or PFO, obtaining a TEE may be needed. It gets a closer look at the left atrium but comes procedural risks.
12.07.2025 20:52 — 👍 0 🔁 0 💬 1 📌 0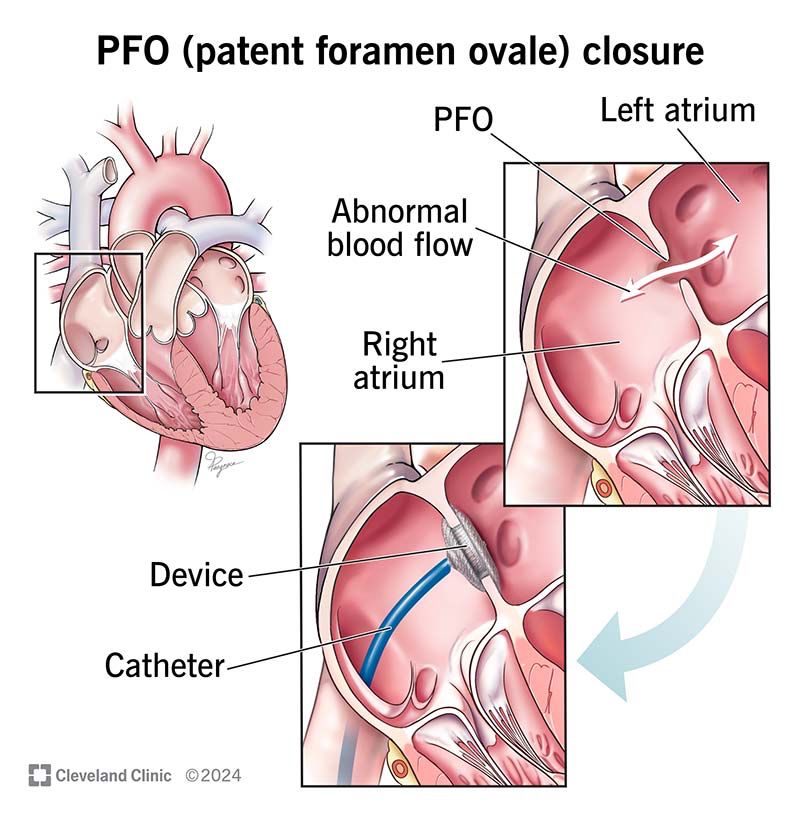
While getting a TTE, we almost always inject agitated saline contrast to look for a PFO. If no PFO is seen, we can usually exclude paradoxical embolus. If we see one, we may have to go DVT hunting in the limbs and pelvis via ultrasound and/or MRV/CTV.
12.07.2025 20:52 — 👍 0 🔁 0 💬 1 📌 0TTEs are good at excluding ventricular thrombi but don’t get a good look at the left atrial appendage (LAA), which is where 90% of clots form in afib.
It can also show chronic atrial disease, low ejection fraction, valvular issues, and other thrombogenic conditions.
DIAGNOSIS
To detect these strokes, we use two types of tools: electrical (EKG with/without ambulatory monitoring) and structural (TTE +/- TEE).
Sometimes you will see strokes of different ages on MRI, suggesting the heart is flinging out multiple clots over a period of time. When these fall in variable vascular territories, it strongly suggests a central (cardio) embolic source.
12.07.2025 20:52 — 👍 0 🔁 0 💬 1 📌 0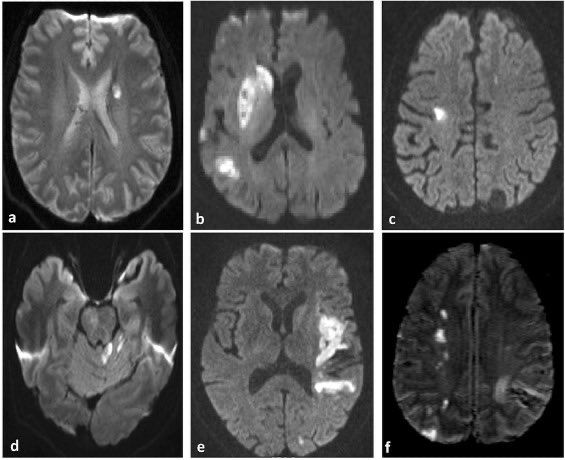
IMAGING
The thrombi from cardioembolic strokes are typically larger than atheroembolic strokes (see pt 1) meaning the strokes generally fall in large vessel territories (not lacunes).
The unique feature is that it can hit any vascular territory, left/right/anterior posterior.
Some of the more important causes include:
- afib/aflutter
- paradoxical embolism via patent foramen ovale (PFO)
- ventricular thrombus
- valvular stenosis
PATHOPHYSIOLOGY
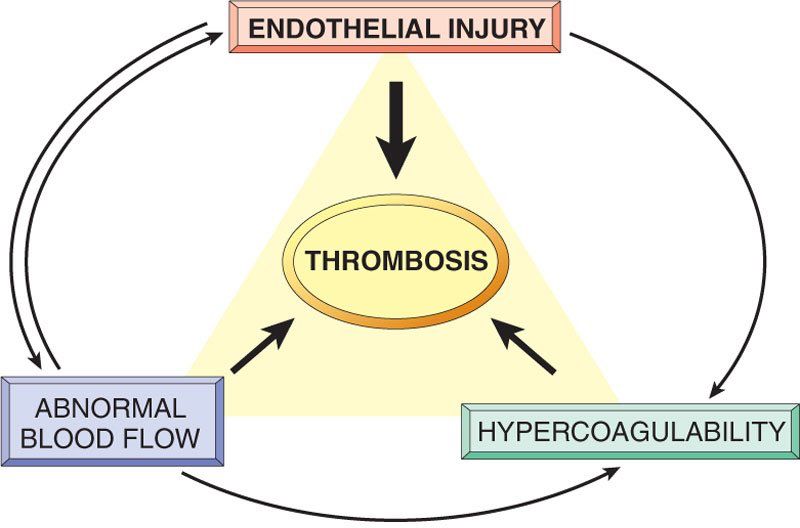
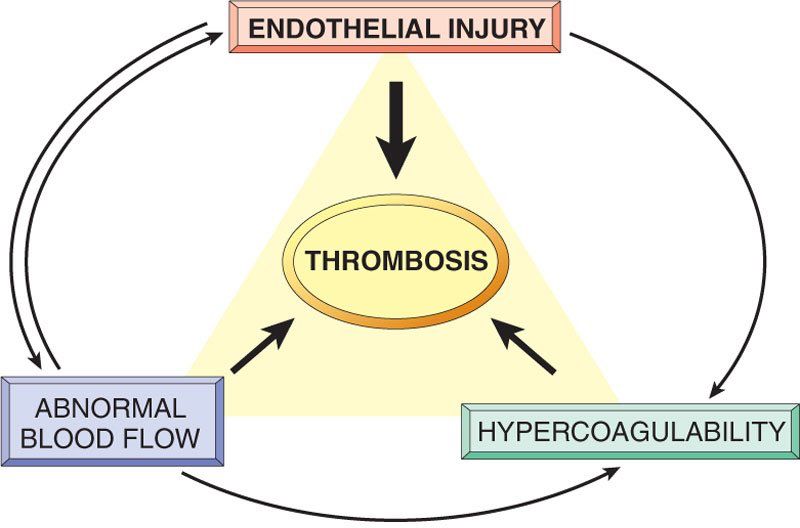
Cardioembolic strokes are generally caused by the other two corners of Virchow’s triad: stasis (eg afib) and hypercoagulability (eg paradoxical embolus from a DVT). Overactivity of secondary coagulation results in a thrombus which can embolize.
INPATIENT STROKE WORKUP
Pt 3: Cardioembolic strokes
In a cardioembolic stroke, a blood clot starts in or passes through the heart but ends up in the brain. It’s managed differently than the other two types we’ve covered. Let’s jump in!
#neurotwitter #neurology #MedEd #FOAMed
My panoptic was money well spent though! I’m trash without it, but I feel pretty good about fundoscopy skills now. I bought it for cheap as an MS4 off of another med student who unwisely bought one before going into anesthesia.
07.07.2025 22:11 — 👍 1 🔁 0 💬 1 📌 0I use mine for pupil assessment. I learned early on that you will never catch subtle anisocoria or an rAPD with a phone light. Need something bright and focused.
07.07.2025 22:09 — 👍 1 🔁 0 💬 2 📌 0Image sources:
1. DOI: 10.1161/01.str.24.1.35
2. DOI: 10.1136/svn-2016-000035
3. DOI: 10.1016/j.jstrokecerebrovasdis.2018.02.010
4. DOI: 10.1001/jamaneurol.2018.1073
5. DOI: 10.1111/nan.12472
6. DOI: 10.1016/j.nicl.2023.103480
7. DOI: 10.1586/17474086.2014.954541
RECAP:
- Acute: lacunar syndromes
- Chronic: vascular dementia
- Imaging: lacunes in the deep white and gray, white matter hyperintensities
- Path: arteriosclerosis and branch atheroma
- Risk factors: HTN, diabetes
- Treatment: antiplatelets, risk factor control
Traditional vascular risk factor mitigation is crucial, most importantly diabetes and hypertension.
These patients are also treated with lifelong single antiplatelet therapy (remember Virchow’s triad).
DAPT has a slight benefit but only in the very short term (ie 21 days).
TREATMENT
Like most ischemic strokes, lacunar syndromes can improve with thrombolytic therapy (ie tPA) in the right time window. By definition, the vessels are too small for thrombectomy, though.
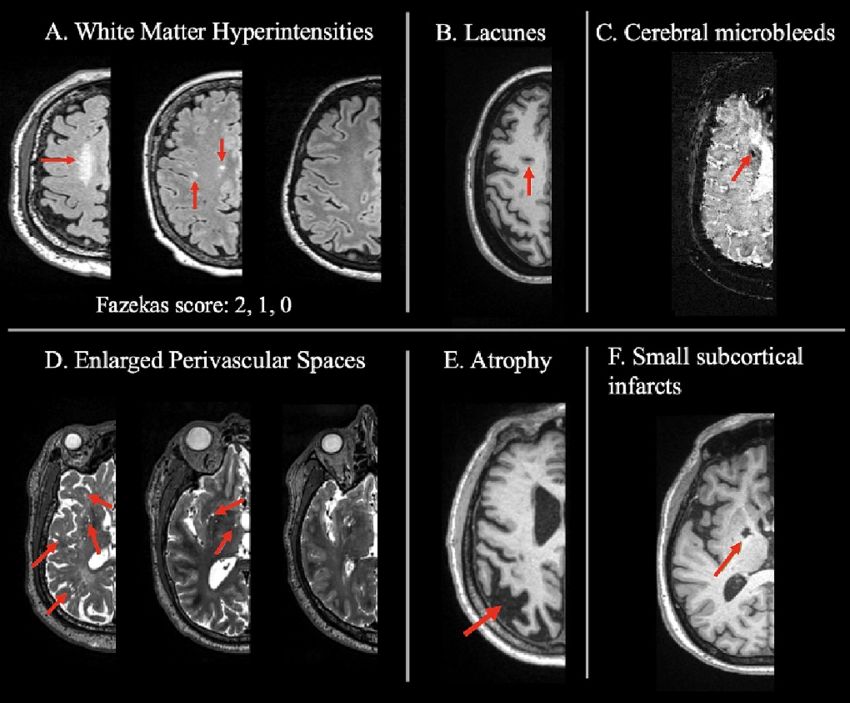
SVD leaves very classic imaging findings, making it easier to radiographically identify:
1. “Holes” of dead tissue (lacunes)
2. Enlarged perivascular spaces
3. White matter hyperintensities (on T2 weighted imaging)
These findings may be too subtle to pick up on CT, though.
It’s more than just an acute problem: chronic SVD can cause subclinical (and eventually clinical) cognitive slowing and is the major contributor to vascular dementia. Imagine it as cognitive damage by 1000 cuts.
07.07.2025 22:06 — 👍 0 🔁 0 💬 1 📌 0Lacunar syndromes usually lack cortical signs such as aphasia, apraxia, and visual field deficits.
But… the thalamus can do almost anything.
Since the strokes are small, recovery is often better and more rapid than for large territory strokes, although this is not a rule.
DIAGNOSIS
SVD presents acutely with some classic lacunar syndromes:
1. Pure motor hemiparesis
2. Pure sensory
3. Ataxic hemiparesis
4. Dysarthria-clumsy hand
5. Sensorimotor
Patients can sometimes present with a “stuttering” course where the stroke worsens over hours to days.
The most important risk factors for small vessel disease (SVD) are hypertension and diabetes mellitus, tobacco use, and cholesterol are all correlated as well.
There are also genetic forms of SVD (CADASIL, CARASIL, others) that are increasingly being recognized.