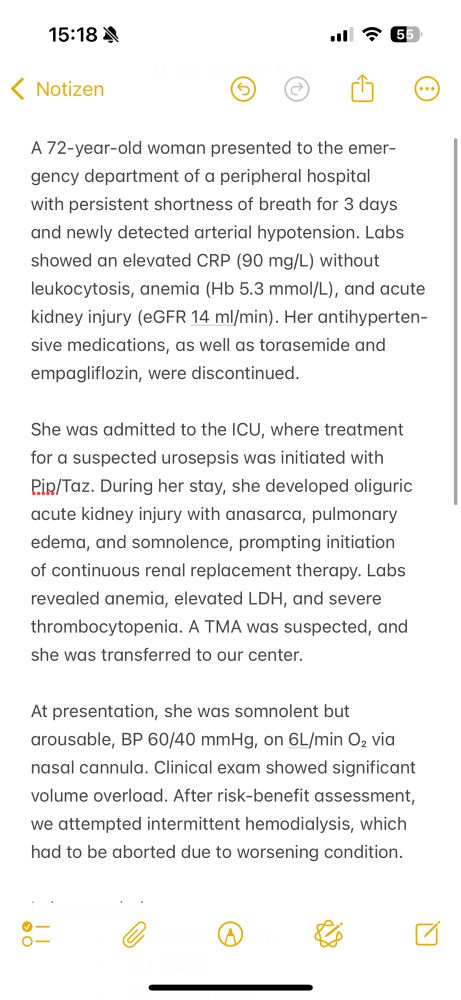
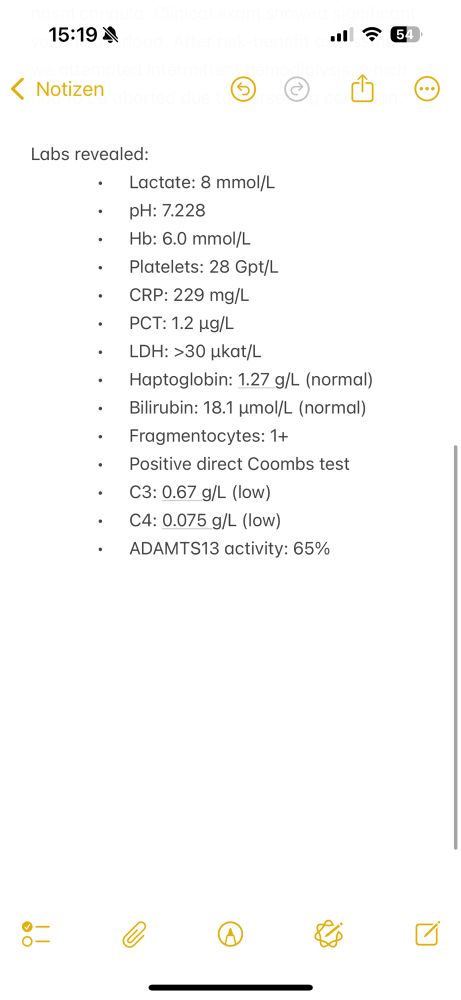
Id like to hear your point of view.
Would you have gone for plasma exchange despite normal haptoglobin/bilirubin and a positive Coombs test?
@renalguy.bsky.social
Nephrology resident at Universitätsklinikum Halle, Germany. Researcher focused on immune deficiency in CKD. Kidneys: the only organs that can throw shade. If they’re salty, you’re in trouble! 😉
Id like to hear your point of view.
Would you have gone for plasma exchange despite normal haptoglobin/bilirubin and a positive Coombs test?
Would love to be added
11.12.2024 18:29 — 👍 0 🔁 0 💬 0 📌 0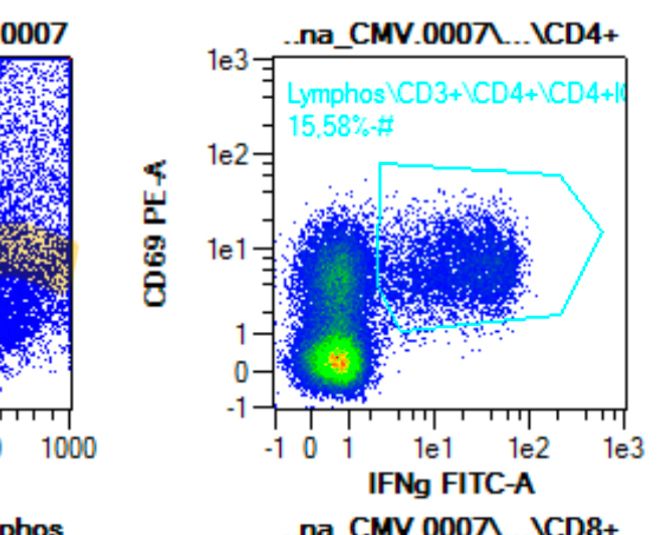
💡 Chronische Nierenerkrankung schwächt das Immunsystem 🛡️ – Proteinurie 🧪 könnte eine Schlüsselrolle spielen. In meiner Doktorarbeit erforsche ich, wie Proteinurie und Immunfunktion zusammenhängen, um neue Ansätze 🩺 zur Risikominimierung und Behandlung zu entwickeln
09.12.2024 21:35 — 👍 0 🔁 0 💬 0 📌 0
ein typischer Tag im Labor: Forschung und Präzision. 🧪🔬 Nephrologie bedeutet nicht nur Patientenkontakt, sondern auch intensive Arbeit im Labor, um die Nieren besser zu verstehen. #Medizin #Nephrologie #Forschung
09.12.2024 08:53 — 👍 0 🔁 0 💬 0 📌 0

Is it too on the nose to bring my colleagues these Christmas cookies shaped like kidneys? Or should I just embrace the nephro-cheesiness? 🎄🍪 #NephrologyLife
29.11.2024 02:13 — 👍 0 🔁 0 💬 0 📌 0Thanks for clarifying! Would you then rely on urinary sodium to differentiate CHF from SIADH? Also, do you find fractional uric acid excretion useful in these cases?
26.11.2024 22:28 — 👍 0 🔁 0 💬 1 📌 0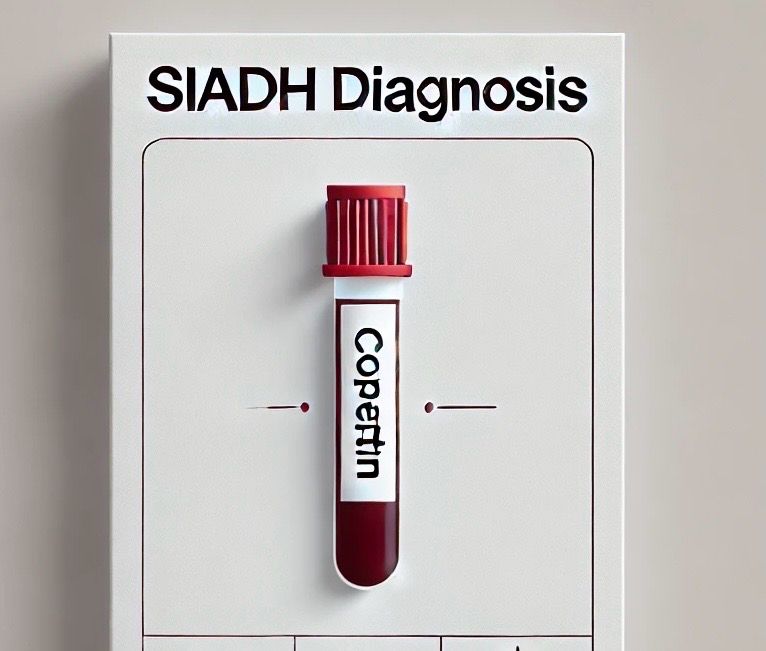
Is copeptin the missing link in diagnosing SIADH, or is it an overhyped biomarker with limited use? How often do you use it for managing hyponatremia? Would love to hear the thoughts of @kidneyboy.bsky.social and @captainchloride.bsky.social !
26.11.2024 21:18 — 👍 0 🔁 0 💬 1 📌 0Thanks for sharing, Joel and Sarah! At my institution, we use xipamide and high-dose furosemide, and if these fail, we escalate directly to CVVHD as we have no experience with 3% NaCl in this setting. How do you decide when to use hypertonic saline?
25.11.2024 18:35 — 👍 0 🔁 0 💬 1 📌 0Thanks, Joel. Sequential nephron blockade sounds comprehensive! Have you had experience combining proximal, loop, and distal tubule blockers simultaneously (e.g., acetazolamide, loop diuretics, and thiazides)? Curious how effective and safe you’ve found this approach
25.11.2024 17:43 — 👍 0 🔁 0 💬 2 📌 0Great point. Do you think there’s ever a scenario where the albumin-furosemide combo is justified, or is it best avoided entirely? Would love to hear your approach in these tough cases
25.11.2024 17:13 — 👍 0 🔁 0 💬 1 📌 0Rituximab in GPA/MPA: 375 mg/m² weekly x4 vs. 1g twice, 2 weeks apart. Is BSA dosing truly better, or does fixed dosing offer equal outcomes with more simplicity? What does your practice prefer?
25.11.2024 15:41 — 👍 1 🔁 0 💬 0 📌 0When diuretics fail, the albumin-furosemide combo is often considered—but is it science or just tradition? Evidence for its routine use is shaky at best. Are we truly helping our patients or just inflating costs and risks?
24.11.2024 22:33 — 👍 6 🔁 1 💬 1 📌 0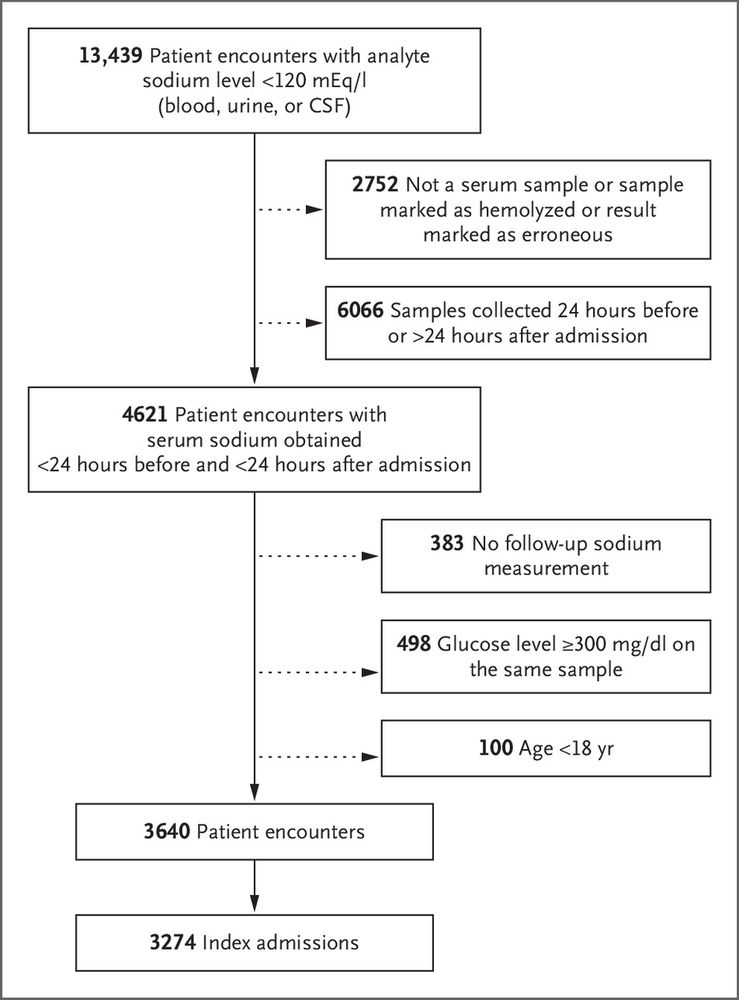
This multicenter observational study recommends a sodium correction of at least 10 mmol/L in patients with severe hyponatremia who have no risk factors. I would be interested to hear Dr. Joel Topf’s @kidneyboy.bsky.social opinion on the matter.
evidence.nejm.org/doi/full/10....