Everyone thinks they are on the side of good.
24.07.2025 15:24 — 👍 0 🔁 0 💬 0 📌 0Anish K Patel
@anishkpatel.bsky.social
‘Just a GP’ posting about general practice and healthcare
@anishkpatel.bsky.social
‘Just a GP’ posting about general practice and healthcare
Everyone thinks they are on the side of good.
24.07.2025 15:24 — 👍 0 🔁 0 💬 0 📌 0Doing docs the other day. So many letters addressed to GPs that have not worked at my practice for 10+ years.
Would this be accepted in any other profession? 🤔

Incentives matter.
And right now, the NHS is still paying people to build bigger spreadsheets, not better systems.
3/3
typeshare.co/anishkpatel/...
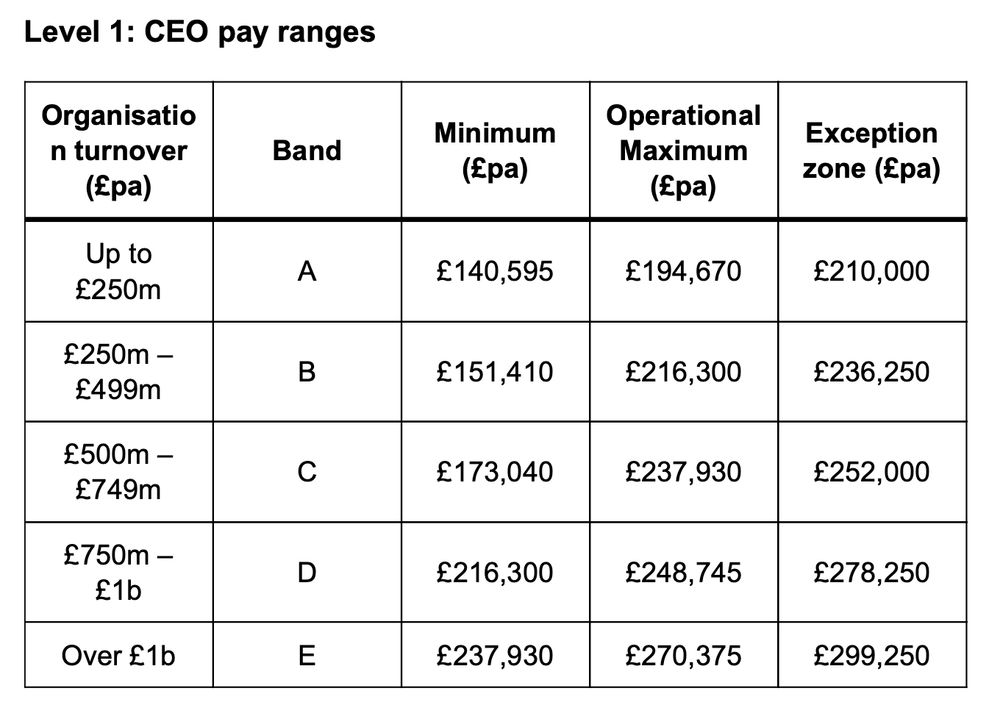
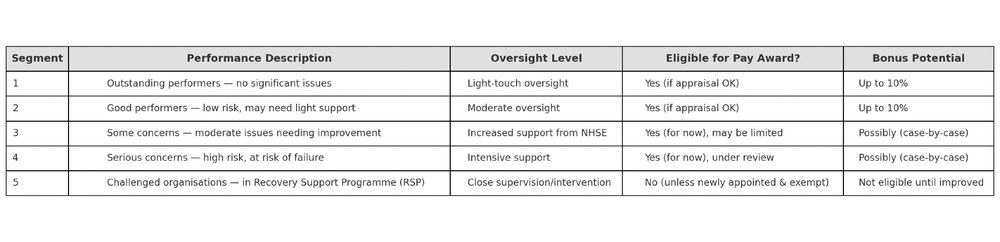
The new 2025 NHS very senior managers pay framework (yes it is called that) tries to shift that.
But it’s still layered on top of a structure that pays for scale, not sense.
Until that changes, the incentives won’t.
2/3
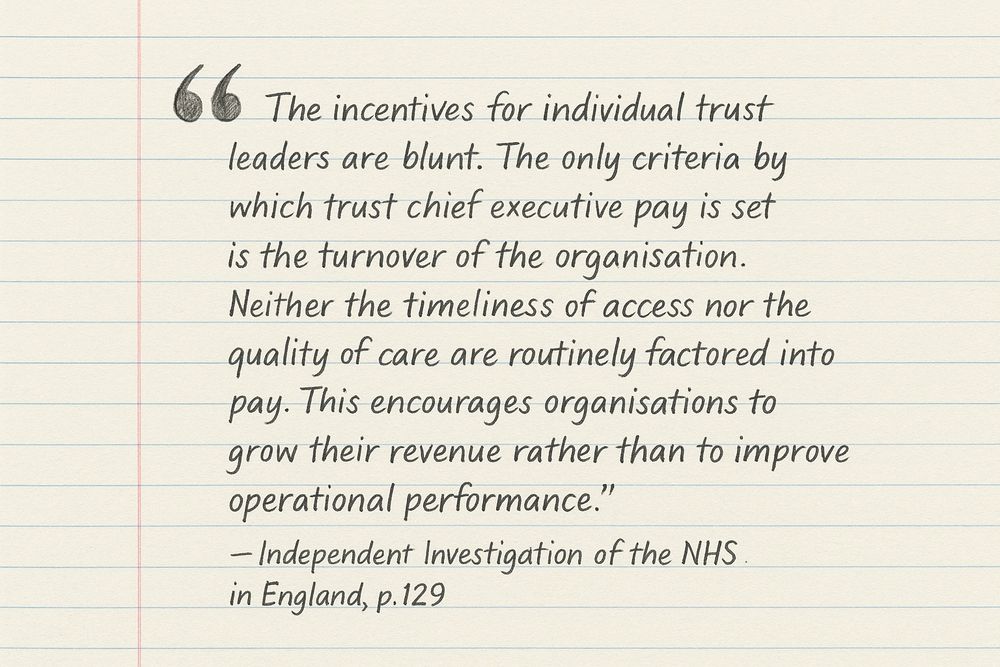
NHS Trust CEOs aren’t rewarded for collaboration.
They’re rewarded for control.
Bigger budget = bigger band = bigger pay.
Even if that means holding on when they should let go.
1/3
Good piece on how it all came about 👇
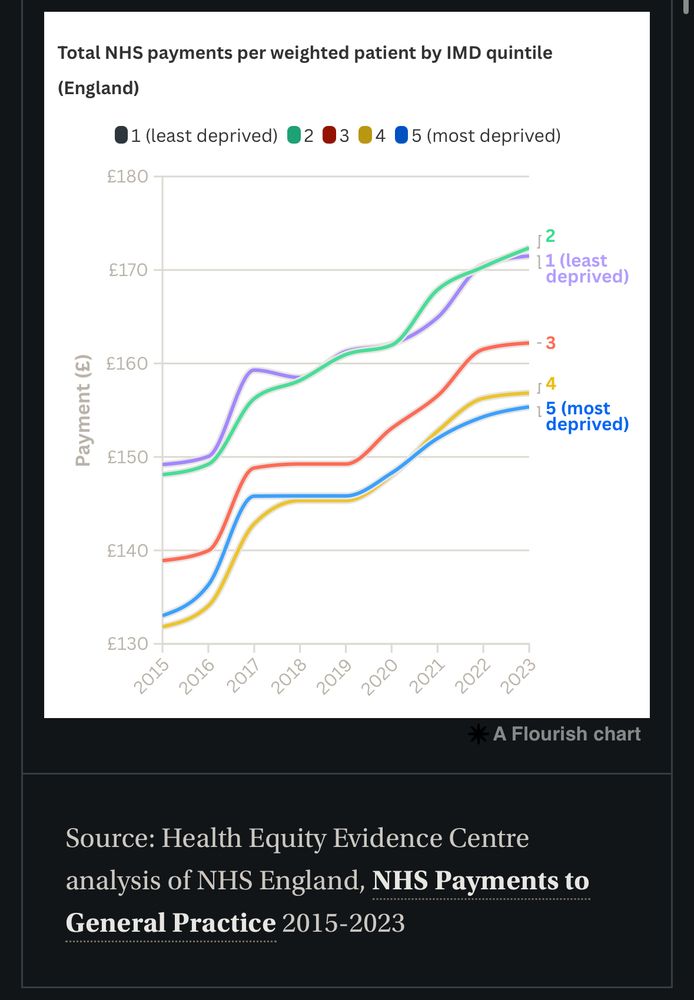
Give you a clue. The Carr-hill formula.
www.nuffieldtrust.org.uk/resource/fai...
I spoke with someone from the voluntary sector while at an ICB event this week. He saw firsthand the gaps in our health and social fabric.
I explained how GP practices in poorer areas actually receive less funding than those in richer ones. His eyes widened. 😳He had no idea.
The hills (that currently feel like mountains) will keep coming.
But remembering the wind at our backs might just make them a little easier to climb.
3/3
typeshare.co/anishkpatel/...
Psychologists call it the headwinds/tailwinds asymmetry.
We notice what holds us back more than what helps us forward.
A problem fixed is quickly forgotten.
We are experts as tracking hardship.
2/3
We talk a lot about what’s going wrong in the NHS. What’s broken. What’s missing.
That’s fair. There’s plenty.
But the danger is we only ever feel the climb.
1/3

The NHS isn’t a machine. General practice isn’t a factory. When we treat it like one, we end up solving the wrong problems. AND create new ones.
3/3
typeshare.co/anishkpatel/...
Data strips out context. It becomes sterile, rigid, and dangerously clean. It flattens messy, human work into neat numbers that are easy to misinterpret and weaponise.
Especially when those at the coal face aren’t the ones holding the spreadsheets.
2/3
Everyone keeps saying better data will fix the NHS. But after years digging into triage and call stats across practices, I’ve realised the opposite is often true.
What gets measured gets misunderstood.
1/3
So we triage. We sort. We see those most in need.
And today, that means you must go elsewhere.
I am sorry. 😔
All I want to do is bring you in.
To sit you down.
To help you—the way we are trained to.
As a team, we handle most of what walks through our doors.
But there aren’t enough of us to go around.
All I can offer now is advice:
• Visit the local chemist, with their rigid list of conditions they’re allowed to treat, or
• Head to the urgent care centre, where you will be seen—but you may wait for hours.
I work through the list, one by one, trying to make the most of what we have to offer.
And now we return to you.
Everything has gone. No more appointments. The end of the road.
I pause over your request.
I come back to you—not because you’re unworthy of my time, but because I must ask:
Is there someone even more in need?
To the Patient I Had to Turn Away 🧵
I see you on my triage list, staring at me.
I see the worry etched across your words. I see the fear.
But I also hear the others calling out just as loudly.
I’ve always treated the patient record with a massive pinch of salt.
AI scribes are the great hope. But a practical coding ability with write back into the EPR is not quite there yet.
Massive bug bear of mine.
Ultimately though comes down to: “the working culture and conditions”.
- When you are taught how to use electronic patient record (EPR) by osmosis
- When people don’t realise how problem codes work, as they never been told
- When you don’t have time to clean things up
Every delay.
Every hoop.
Every added task with no time to do it.
It’s not a glitch.
It’s a structure that drains the people it relies on.
We don’t burn out by accident.
We burn out by design.
typeshare.co/anishkpatel/...
It should be the most meaningful job in the world.
You help people when they’re scared, broken, or lost.
But instead of feeling fulfilled, you feel empty.
This is what burnout in the NHS really feels like.
And it’s not just happening.
It’s being designed into the system.

Don't hold back Doncaster LMC:
"The latest changes to the GP contract for 2025/26, as outlined by the BMA, are yet another disappointment for general practice.”
www.doncasterlmc.co.uk/the-2025-26-...

Trying something new – creating YouTube videos. Turns out talking to a camera is way harder than it looks, but I’m giving it a go. First up: how NHS GP funding is rigged against poorer areas. Let’s see how this goes… 🎥👇
youtu.be/D-oXS45gIbA
The real Q is: Will those in power fund a safe and sustainable general practice?
We’ll find out in the 10-year NHS plan
📊 The Gold Standard: 1 GP per 1,000 pts
📈 The need: 2,859 FTE GPs per year
🎓 The pipeline: 6,000 GP Regs per year by 2031
💰 The missing piece: Funding
[End]
A Choice
This can be fixed
If we commit to funding new GP posts, we can:
✅ Make sure practices can afford to hire GPs
✅ Improve retention by spreading workload fairly
✅ Stop the brain drain to other countries
This is not a fantasy. The numbers do work.
The Global Competition
GPs are in demand worldwide. Canada, Australia, and New Zealand offer better pay, better working conditions, and a better work-life balance.
We are already training many of the world’s GPs. Do we want to keep them, or export them?
Adding 1️⃣+2️⃣ = The Freezing of GP Posts
A dangerous trend is emerging: as GPs leave, many practices will freeze their positions. Not because they don’t need a replacement, but because they can’t afford to hire one while keeping the lights on.
2️⃣ Hiring: A Funding Crisis
Another problem has emerged: qualified GPs can’t find jobs. It sounds absurd—we need more GPs, yet practices can’t afford to hire them. It is a failure to fund GP posts.