Congratulations to all the Interns of this new program! Looking forward to follow their journey.
21.06.2025 15:08 — 👍 3 🔁 0 💬 0 📌 0
Legends!
10.05.2025 16:27 — 👍 1 🔁 0 💬 0 📌 0
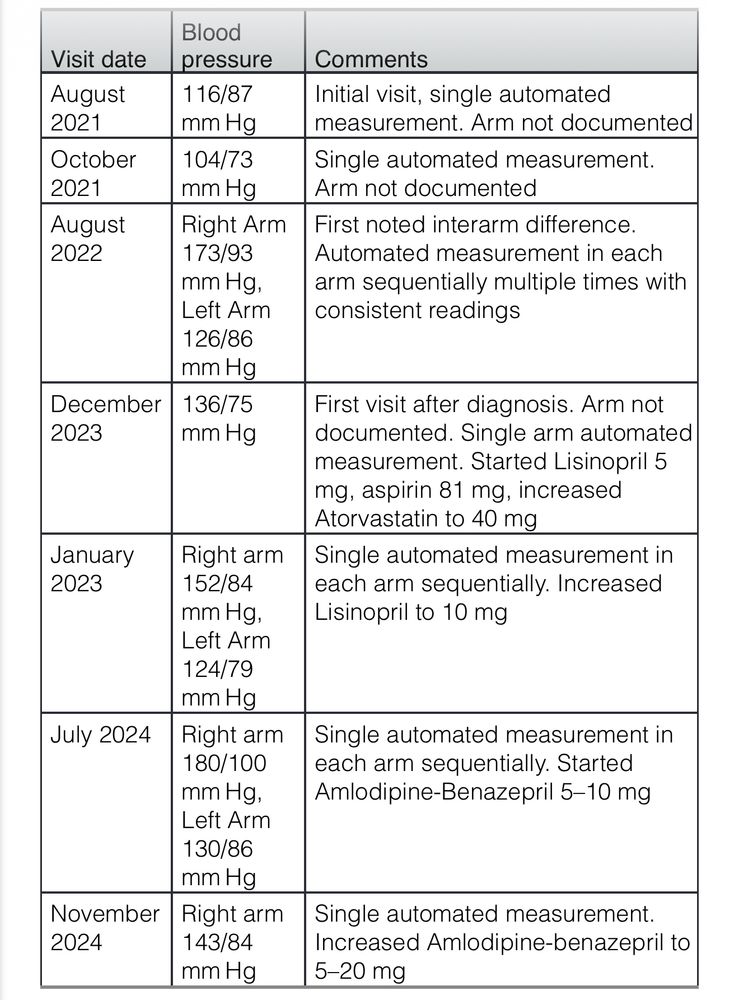
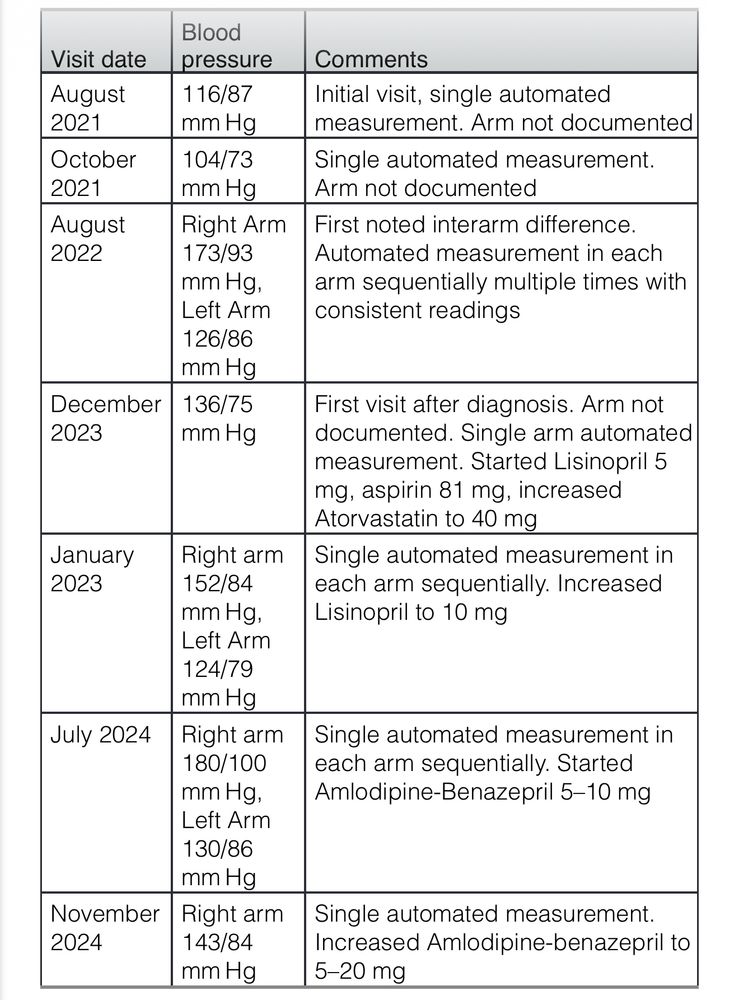
Table. Timeline of Clinic Visits and Blood Pressure Measurements
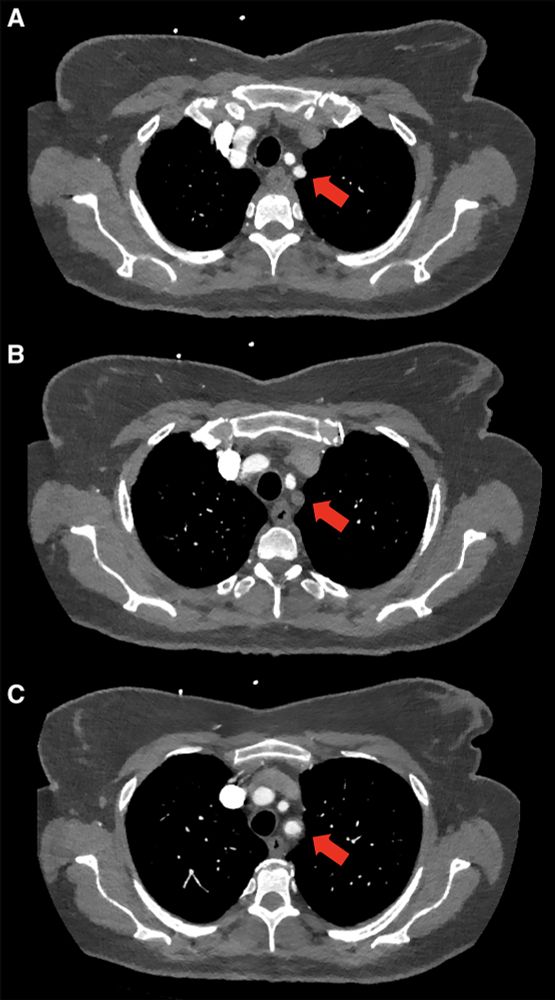
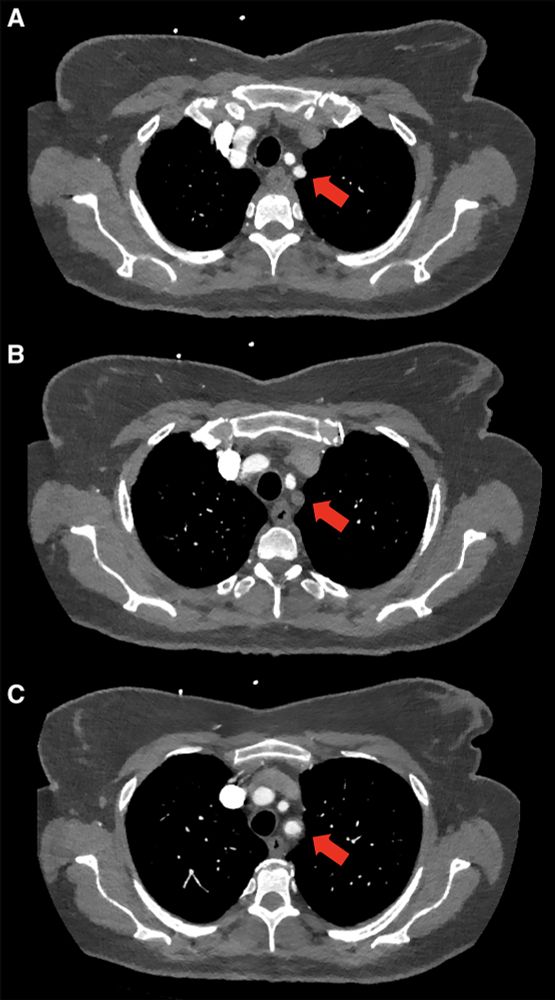
Figure. Computed tomography angiography (CTA) of subclavian artery stenosis. Axial CTA image of this patient with subclavian artery stenosis. A, Patent subclavian artery (indicated by the arrow) distal to the site of the occlusion. B, A more inferior axial image with an absence of contrast in the subclavian artery at the level of the subtotal occlusion while (C) demonstrates the most inferior and proximal to the aortic arch and re-demonstrates a patent proximal portion of the subclavian artery. This is consistent with a subtotal occlusion of the subclavian artery with distal reconstitution likely via the left vertebral artery
A one year delay in diagnosis of #hypertension!
Clear illustration of the importance of measuring BP in both arms
www.ahajournals.org/doi/10.1161/... in @ahajournals.bsky.social Hypertension
24.04.2025 23:56 — 👍 32 🔁 10 💬 1 📌 0
This. 😇
17.04.2025 09:21 — 👍 0 🔁 0 💬 0 📌 0
Not lastly, #NephSky #MedSky
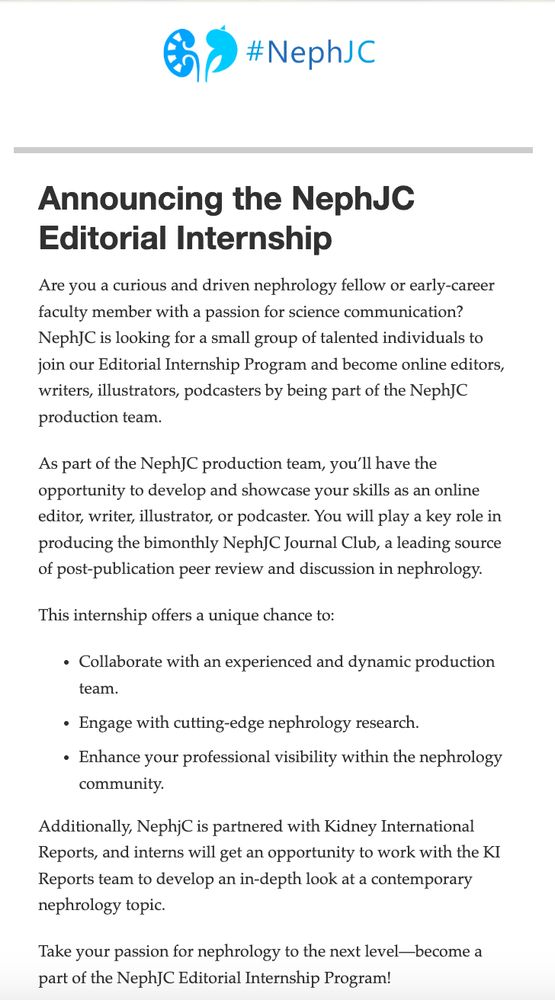
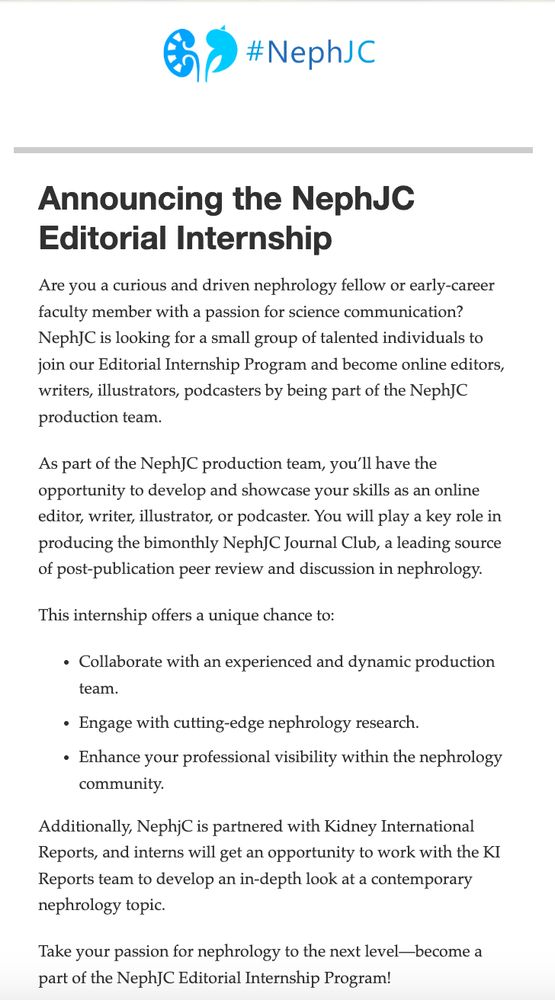
✨This year we try something new: #nephjc internship
If curious, wanna apply, need to be part of our world-wide community, apply 👇
12.03.2025 02:03 — 👍 13 🔁 7 💬 0 📌 0
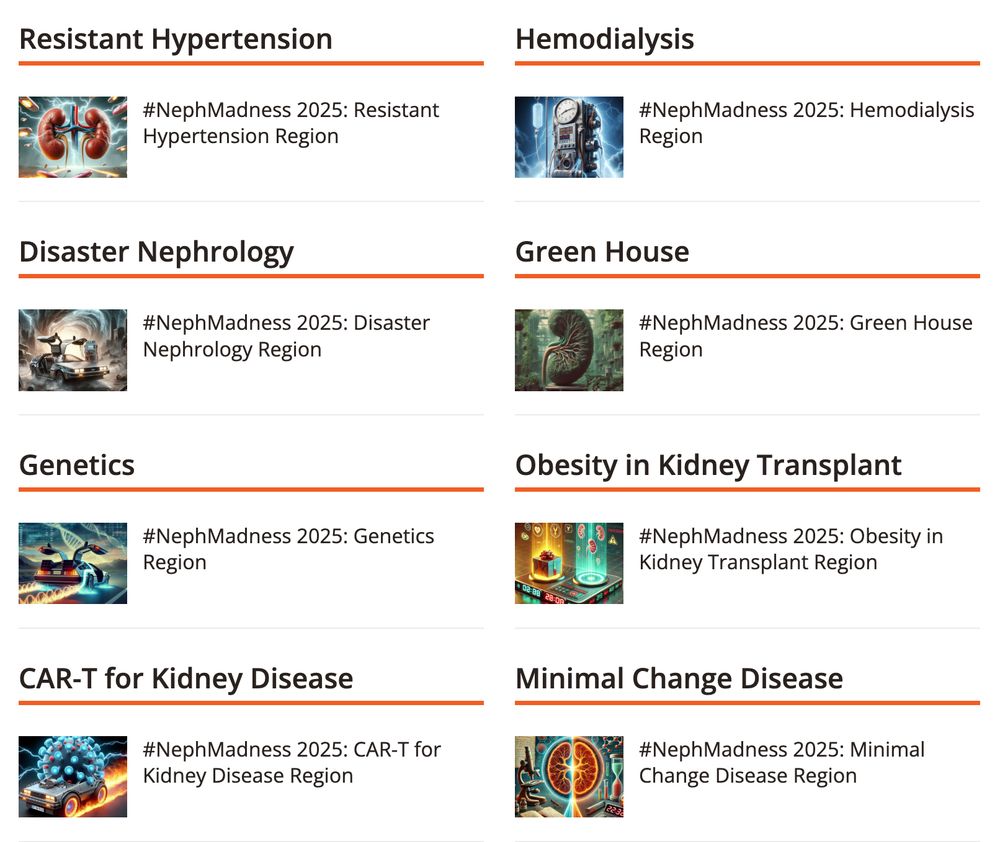
Need weekend plans?
Catch up on all the #NephMadness 2025 regions:
-Resistant Hypertension
-Obesity
-Green House
-Minimal Change Disease
-Disaster Nephrology
-Genetics
-Hemodialysis
-CAR-T for Kidney Disease
Happy reading!
bit.ly/4iMNijV
15.03.2025 16:00 — 👍 6 🔁 2 💬 0 📌 0
I order it in resistant hypertension or young patients with hypertension. I admit I have a wonderful endocrinologist team who helps me interpret results and go further with more tests if necessary.
26.02.2025 17:19 — 👍 2 🔁 0 💬 0 📌 0
That’s where I am coming from. Thank you for your input on this.
20.02.2025 18:07 — 👍 0 🔁 0 💬 0 📌 0
Do this interfere on your decision making? Having proteinuria <1 gr or >2 gr can make a difference in some patients.
20.02.2025 17:08 — 👍 0 🔁 0 💬 1 📌 0
That’s a very good point. Thank you.
20.02.2025 07:08 — 👍 0 🔁 0 💬 1 📌 0
Thank you very much. Very helpful! 🙆🏽♂️
19.02.2025 18:46 — 👍 0 🔁 0 💬 0 📌 0
Now that we are in the subject, do you have any specific use for Cr excretion? Do you consider any specific value for “high” and “low” or just go with what your lab parameters?
19.02.2025 14:58 — 👍 0 🔁 0 💬 1 📌 0
I’ll take a look. Thank you very much!
19.02.2025 14:55 — 👍 0 🔁 0 💬 0 📌 0
BMI > 30 but no hyperflitration in eGFR.
19.02.2025 14:18 — 👍 0 🔁 0 💬 1 📌 0
Correlación entre el cociente proteína/creatinina en orina esporádica y las proteínas en orina de 24 horas
All I found was this study, which concludes that there is a strong correlation between both tests. In my clinical practice, this is not the case. I want to hear everyone’s thought on this. Here to learn!
www.revistanefrologia.com/es-pdf-X0211...
19.02.2025 09:15 — 👍 0 🔁 0 💬 0 📌 0
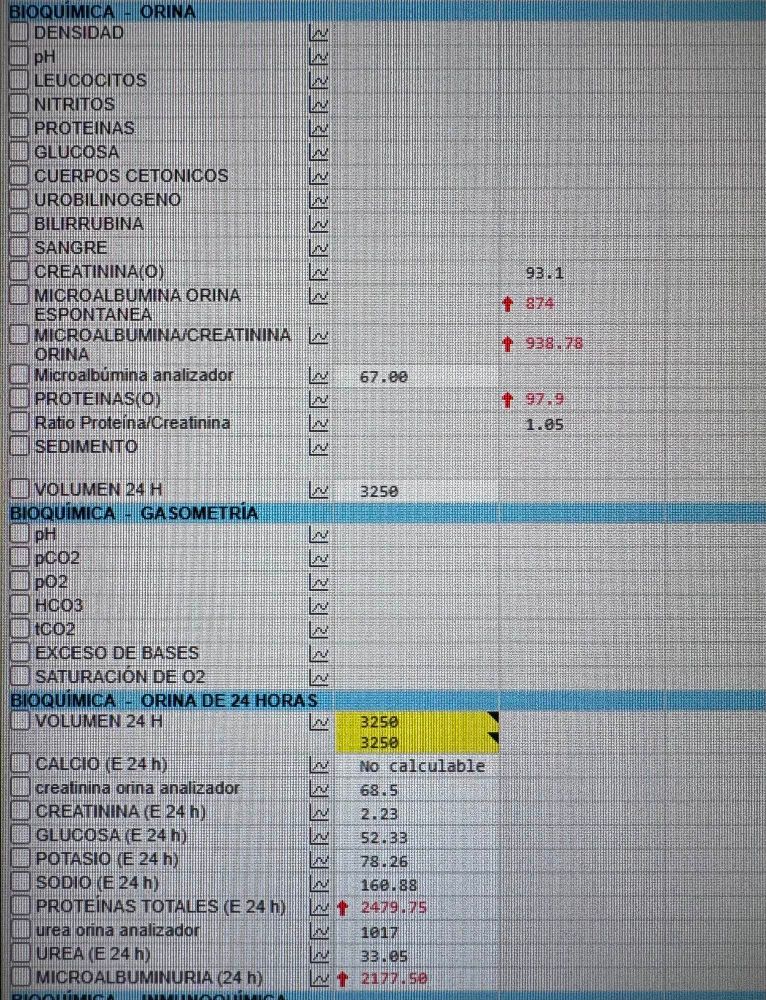
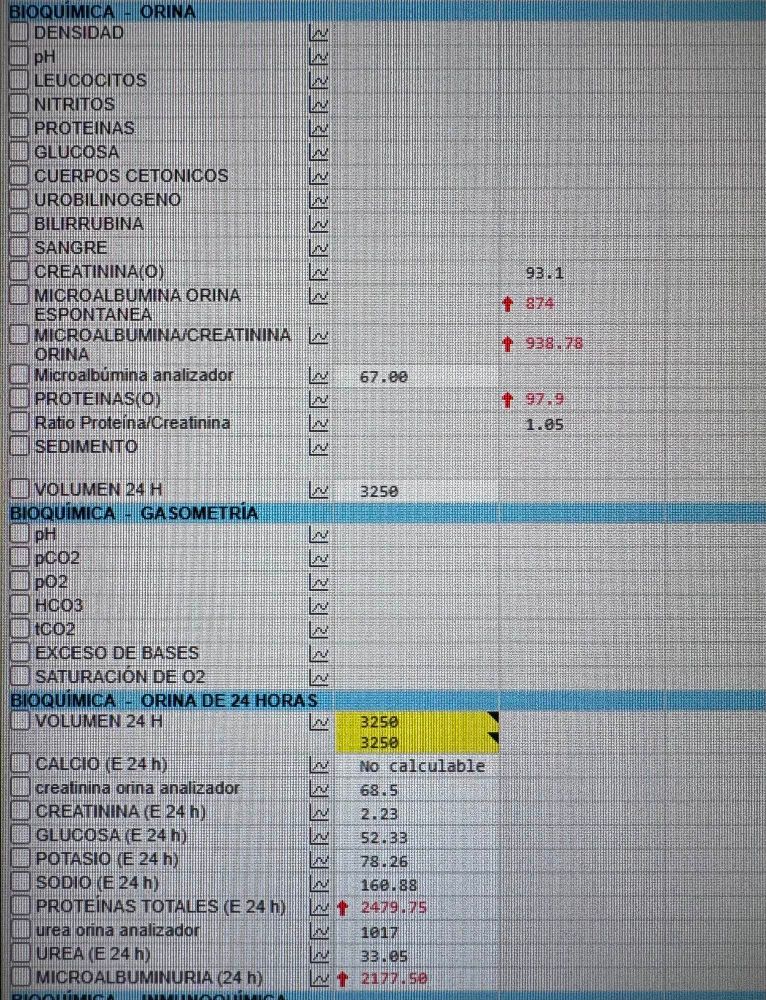
A question to all Nephrologists, how do you approach the difference in proteinuria between samples of spot urine and 24 hr urine?
In this example:
- Spot Urine Alb/Cr ratio: 938 mg/g
- 24 hrs: 2,177 mg/24 hrs
My calculations for Alb/Cr ratio in 24 hr is 985 mg/g
#AskRenal
19.02.2025 09:12 — 👍 3 🔁 1 💬 3 📌 0
🤩
18.12.2024 08:58 — 👍 0 🔁 0 💬 0 📌 0
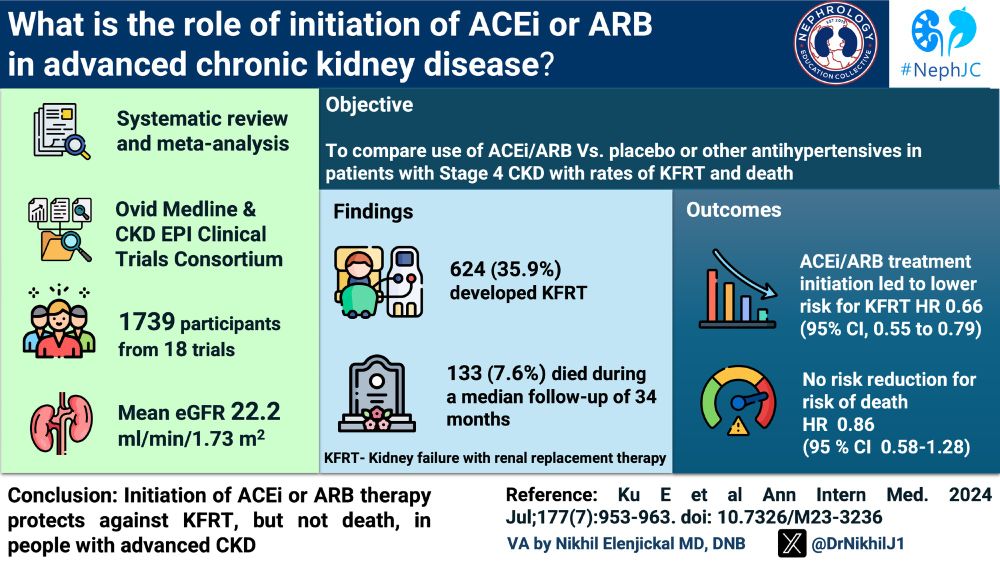
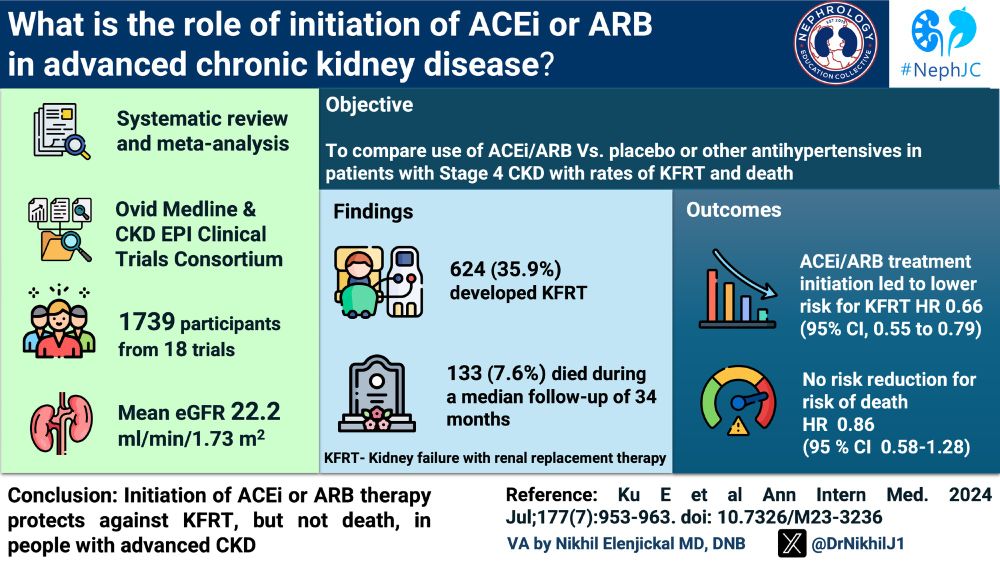
🎨The visual abstract made by @drnikhil.bsky.social
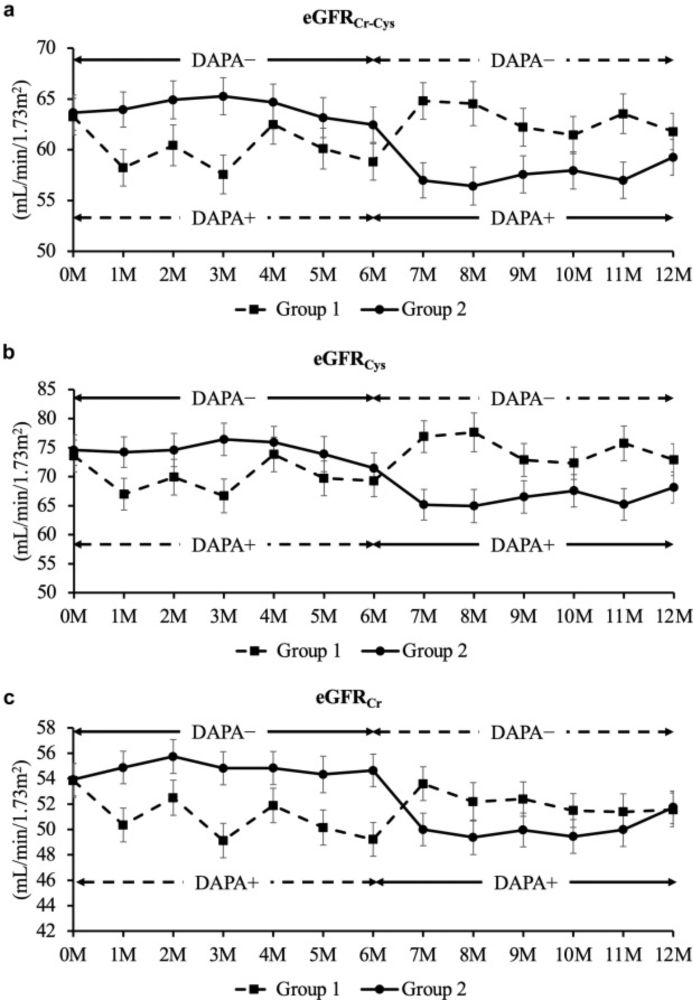
#NephSKy #MedSKy, tonight #NephJC goes with an oldie but still goldie topic: RASi in advanced CKD
⏰ Same hour, 9 pm EST
www.nephjc.com/news/2024/12...
17.12.2024 14:38 — 👍 20 🔁 11 💬 0 📌 0
Thank you for the insight @jamiekwillows.bsky.social , it definitely spiced up the discussion. And thank you to all the @nephjc.bsky.social team for having my back on this one. I deeply appreciate it and feel flattered to have the opportunity to participate.
17.12.2024 13:33 — 👍 4 🔁 0 💬 0 📌 0

ACEing the management of advanced CKD — NephJC
This week we come to meta-analyse, strikingly late, the cornerstone of all CKD treatments. Are you still in doubt? We need ACEing CKD to the end of GFR, and beyond
Afraid of RASi on advanced CKD? Should we initiate ACEi and ARBs in stage 4 CKD? Is it safe? Is it worth the risk? Find the answers in this week’s #NephJC blogpost about the most recent meta-analysis on the subject.
Spoiler: Keep Calm and Aceit!
www.nephjc.com/news/aceing-...
17.12.2024 12:51 — 👍 3 🔁 0 💬 0 📌 0
This is the way.
07.12.2024 18:43 — 👍 1 🔁 0 💬 0 📌 0
Yeah. I would.
05.12.2024 14:39 — 👍 0 🔁 0 💬 0 📌 0
I wouldn’t mind doing my Residency again 😅.
04.12.2024 21:17 — 👍 1 🔁 0 💬 1 📌 0
Thanks for sharing.
30.11.2024 08:00 — 👍 2 🔁 0 💬 0 📌 0
Thank you.
29.11.2024 10:00 — 👍 0 🔁 0 💬 0 📌 0
I understood that a solute is or not an effective osmole not because of its ability to permeate a cell membrane but it’s a ability to create a gradient by “dragging water”. Am I wrong about this?
Saying urea isn’t an effective osmole is confusing to me, because of desequilibrium syndrome.
28.11.2024 10:16 — 👍 1 🔁 0 💬 2 📌 0
MD FASN | Nephrologist = kidney doc | #PeritonealDialysis aficionado | #ClinicianScientist @ChariteBerlin | Editorial fellow @JASN | #SingleCell | Determined to understand adaptation to kidney disease | #ERCStG
Practical handbook of kidney diseases. Just-in-time information when and where you need it. https://apple.co/454QweZ. Editors: Mark Rosenberg & Sandeep Gupta
Molecular Psychiatry, Neuroscience, Genetics, Professor at Karolinska Insitutet
Nephrologist in Mexico, HGM, #NSMC intership 2024 #NephSky #MedSky #LatinSky #HMSky #Kidneydisease #sunrise #NephJC
🇵🇪 MD from Cayetano Heredia | Research scholar at UAB | Aspiring to IM and nephrology 🦥 | Evidence based medicine📍| Feminist | she/her | #MedSky
Assistant professor of Nephrology in Santhiram Medical College, Nandyal
Passionate in Preventive Nephrology and Critical Care Nephrology
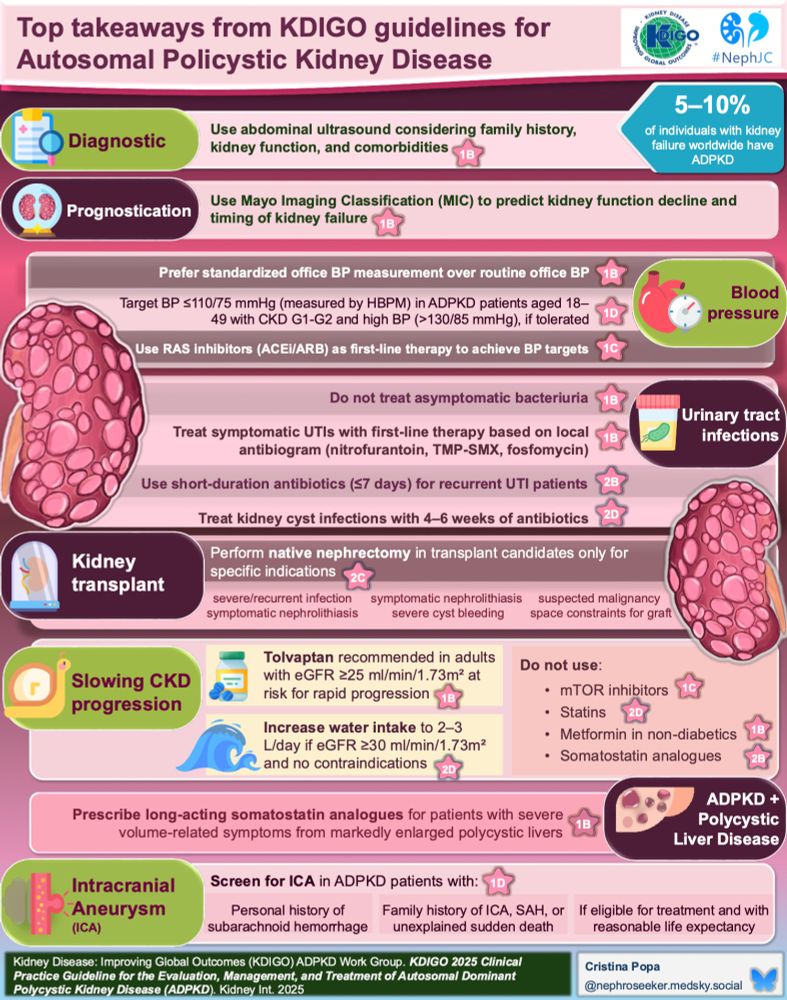
I'm a young nephrologist from Iași, România, currently doing my phd on ADPKD and started an internship at #nephjc
Pharmacist | Clinical Professor
✨Interest in Nephrology Medicine #NephJC #NephSky
Curious nephrologist navigating the ever-evolving world of kidney care. Learning, connecting, and growing every day—one nephron at a time.
Assistant Professor of Medicine, UofR
Nephrologist by Day / Muggle by night
MD Internal Medicine, PGI Chandigarh
DM Nephrology, CMC Vellore, India 🇮🇳
Passionate nephrologist ! 🩺 👩🏻⚕️
Perspicacious toddler mom ! 👩🏻🍼
Nephrologist , transplant physician
2x Kidney/Pancreas Transplant Recipient, Research Collaborator, Medical Science Liaison- Solid Organ Transplant, Nephrology, Infectious Disease, Hepatology
(he/him)
Neurodivergent Social Democrat in Maine working to build a diverse, equitable, and inclusive society.
Economist by training, Spanish-English-American by birth, and antifascist by moral imperative.
We must act now before it is too late.
Clinical Fellow | Nephrology | SCO | Manchester
"Thoughtfully Create Really Excellent Input"
Interventional Nephrology, ULS São João
#POCUS #VascularAccess #CardioRenal
Nephrologist in training at university hospital Mainz
NephJC Intern 2025