We lost an icon today! Activist, scientist, and a difficult woman! #JaneGoodall
01.10.2025 23:22 — 👍 5 🔁 0 💬 0 📌 0@docnessmonster.bsky.social
Pain rerouted my life - so I made it my work. Neuro nerd. Chronic illness realist. I believe rest is power, science is for everyone, and the body knows more than we’re taught to trust.
We lost an icon today! Activist, scientist, and a difficult woman! #JaneGoodall
01.10.2025 23:22 — 👍 5 🔁 0 💬 0 📌 0
Our final contribution to this collaboration is now online. We obtained electrophysiological recordings of DRG/TG neurons and Fos+ neurons of spinal dorsal horn & vlPAG in 2 models of neuropathic pain to study the actions of a humanized P2X4R scFv #PainResearch www.sciencedirect.com/science/arti...
17.09.2025 17:00 — 👍 5 🔁 1 💬 0 📌 0Keyword: Dudes? I would love to see more non-men (including women, non-binary, intersex, etc scientists) receive the top prize.
12.09.2025 19:32 — 👍 0 🔁 0 💬 0 📌 0
⚡We are finally electrocuting DRG neurons in the @alleslab.bsky.social since moving to @cincychildrens.bsky.social! #PainResearch #ephys #NeuroSkyence
10.09.2025 17:50 — 👍 14 🔁 1 💬 1 📌 0Congrats! I would love to talk with you one on one about what it's like to do research in Poland! Sent you a message on LinkedIn!
08.09.2025 17:02 — 👍 1 🔁 0 💬 0 📌 0🧪Biomarkers in a clinical setting for Alzheimer’s! Scientific work in identifying biomarkers for all sorts of health conditions leads to faster diagnosis, informs treatment, and improves health!
04.09.2025 22:14 — 👍 2 🔁 0 💬 0 📌 0🔍How do we test for biomarkers?
Usually through blood samples - looking for proteins, cytokines, or other molecules.
It's still early days in the pain field, but blood-based biomarkers may one day help personalize pain treatments.
#HealthResearch #ChronicPain
🧪Word of the Week: Biomarker
A measurable signal in the body, like a molecule in the blood, that tells us something about health, disease, or response to treatment.
For pain, biomarkers could help make the invisible visible, giving us ways to track or predict pain.
#SciComm #PainResearch
This! If you read the paper they also were able to ID potential therapeutics based on the biomarkers. Spoiler, the therapeutics were not traditional analgesics. Though something like this is years (maybe even decades) from the clinic, this is huge first step!
30.08.2025 13:20 — 👍 2 🔁 0 💬 0 📌 0
A blood test for pain?
New work in Nature identifies circulating biomarkers that distinguish chronic pain states—offering a path toward objective, biologically grounded diagnostics.
#PainResearch #Neuroskyence #Biomarkers #ScienceWatch #SciComm #ScienceInTranslation #ChronicPain
Doing my best to get better at this! You will see more and more from me as I try to communicate what we do, how we do it, and what it all means! Hoping to reach not just the science folks here on BS but non-scientists as well!
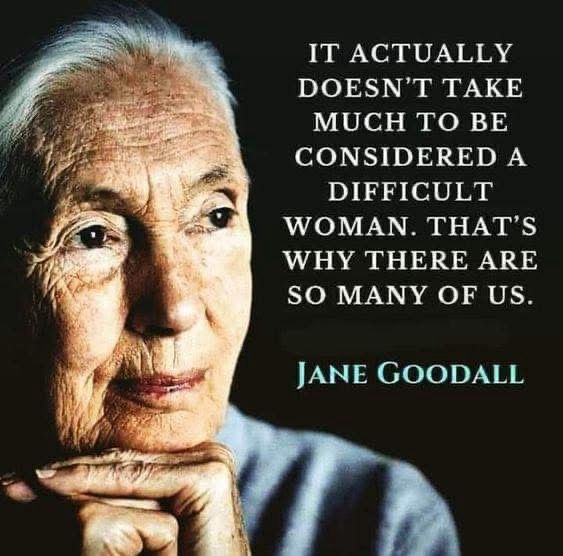
27.08.2025 21:11 — 👍 5 🔁 1 💬 0 📌 03/ DRG are where sensory neurons, including nociceptors, send their signals to the spinal cord.
27.08.2025 18:32 — 👍 2 🔁 0 💬 0 📌 0
2/ Here is what the human spinal cord and real DRG look like in humans! Image from human donor and our journal cover in www.jpain.org/article/S152.... White arrows show the DRG, the same clusters shown in the cartoon above.
27.08.2025 18:30 — 👍 3 🔁 0 💬 1 📌 0
1/ Word of the Week: Dorsal Root Ganglia (DRG)
Clusters of nerve cell bodies (soma) near the spinal cord that relay sensory signals - including pain - from the body to the brain.
Curious what they look like in real human tissue? See thread below
#NeuroSkyence #PainResearch #ChronicPain #SciComm

One of our final papers from this collaborative effort involving collaborators at UNM, Mayo Clinic, & McGill. Here we validate a humanized scFv targeting hP2XR. Kudos to first-author @docnessmonster.bsky.social & former lab member Mark S. for making this happen! journals.sagepub.com/doi/10.1177/...
26.08.2025 12:37 — 👍 2 🔁 2 💬 0 📌 0
6 📖 Read the full study here! www.jci.org/articles/vie...
22.08.2025 15:20 — 👍 0 🔁 0 💬 0 📌 05/ 💡 Toward personalized care:
The study shows that inflammation is the earliest shift in diabetic nerve damage.
Controlling it early may prevent the cascade.
This opens a window for preventive intervention.
4/ 🧠 Why it matters:
This work reveals a progressive cascade:
🧱 Perineurial disruption →
🔥 Immune infiltration →
🧵 Fibrotic remodeling →
📉 Schwann cell loss
Each stage offers a window for intervention.
3/ 🧬 What did they find?
Inflammation dominates: IL6, IL1B, CXCL2 were upregulated in DPN nerves
Fibrosis follows: TGF-β and Tenascin signaling increased in late-stage axonal loss
Sensory nerves are hit hardest, especially the sural nerve
2/ 🔬 What did they do?
The team collected human tibial and sural nerves from patients with and without diabetic peripheral neuropathy (DPN).
Using bulk and spatial transcriptomics, they mapped gene activity and tracked inflammation, cell types, and axonal mRNA transport.

Infographic titled "From Lab To Life: How Diabetes Rewires the Peripheral Nervous System – And what that means for treatment?" It is divided into four sections. The first section, "The Challenge," explains that about 50% of diabetes patients develop diabetic peripheral neuropathy (DPN), which causes pain, numbness, and disability, and highlights the lack of understanding of nerve degeneration. The second section, "What they did?" describes how researchers collected human tibial and sural nerves and used spatial transcriptomics to map gene activity and track inflammation and mRNA transport. The third section, "What they found?" reports increased inflammation markers (IL6, IL1B, CXCL2) and fibrosis markers (TGF-B, Tenascin) in DPN nerves. The final section, "Why it matters?" emphasizes the potential for early intervention to prevent fibrosis and axonal loss, moving toward personalized care. Visuals include a leg with pain indicators and a nerve illustration showing inflammation. The study is credited to Tavares-Ferreira et al., J Clin Invest, 2025, with a DOI link.
🧠From Lab To Life
Why do peripheral nerves suffer axonal loss in diabetes?
A study led by @dianatavf.bsky.social from the @tedpricethepainguy.bsky.social lab showed how inflammation leads to neural fibrosis in diabetic peripheral neuropathy! #PainResearch #Neuroskyence #FromLabToLife 1/

Three lab members standing proudly in front of a newly assembled electrophysiology rig. The setup includes a micromanipulator, amplifier, and monitor, with cables neatly arranged. Everyone is smiling in casual lab attire, celebrating the milestone in a well-lit lab space.
📸 Big day in the lab!
Our new electrophysiology rig is officially up and running — huge thanks to everyone who helped make this happen. Excited for the science ahead! 🧠⚡️
@alleslab.bsky.social @cincychildrens.bsky.social #PainResearch
This work is finally online as in-press preview!
JCI - Cell and molecular profiles in peripheral nerves shift toward inflammatory phenotypes in diabetic peripheral neuropathy www.jci.org/articles/vie...

FlyBase, a Drosophila database, will lose a third of its team in early October because the Harvard grant that covered the employees’ salaries was canceled. Scientists warn that losing FlyBase could devastate fly research.
By @claudia-lopez.bsky.social
www.thetransmitter.org/community/ha...
🔬 Very cool work from @aubinmoutal.bsky.social, @khannalabuf.bsky.social, and team! These studies reveal how auto-antibodies—like those seen in autoimmune diseases—can directly target sensory neurons in the dorsal root ganglia, driving painful neuropathies. #PainResearch
11.08.2025 13:50 — 👍 2 🔁 0 💬 0 📌 0
This is a step toward truly personalized pain treatment — the kind that adds life to the years for people living with neuropathic pain.
🧠💜 Deep thanks to the donors and families who make this work possible. 4/4
pubmed.ncbi.nlm.nih.gov/40657722/
In one donor, gabapentin calmed down hyperactive neurons and reversed abnormal gene activity - especially in pathways tied to inflammation and ion channels.
We’re not just studying how gabapentin works - we’re learning who it works for and why. 3/4
We paired patch-clamp electrophysiology with gene expression analysis and found that gabapentin’s effects were tied to both the type of neuron and the donor's unique biology.
The science is complex, but the takeaway is simple:
Gabapentin’s pain relief isn’t one-size-fits-all. 2/4

Alt text (expanded version for web or accessibility-focused platforms): Vertical infographic titled “Why Gabapentin Works Differently for Different People.” Section 1 explains that 10% of adults live with neuropathic pain and gabapentin doesn't help everyone. Section 2 shows that researchers used donated human dorsal root ganglia (DRG) neurons to study gabapentin’s effects, combining electrophysiology and RNA sequencing. Section 3 illustrates how gabapentin reduced excitability in some donors’ neurons but not others, and those differences matched gene expression profiles. Section 4 highlights how this could lead to more personalized pain treatment that adds life to the years of people living with chronic pain. Footer credits the donors and includes the study DOI
Gabapentin is widely prescribed for nerve pain, but it doesn’t work the same for everyone.
We studied actual human sensory neurons from donors and found that some responded strongly - and others hardly at all.
#fromlabtolife #neuroskyence #PainResearch 1/4
That being said novel research shows Tylenol effects Nav1.7/1.8 currents so these targets are still therapeutic targets. I believe data from the Waxman lab showed specific areas of NaV1.7 are responsible for specific pain syndromes. Perhaps that may help ID new drugs for NaV1.8 🤔
06.08.2025 00:29 — 👍 1 🔁 0 💬 0 📌 0