1/ It’s been a struggle to process what happened at the CDC just a few days ago. The facts are coming in: one officer died, 500 rounds fired, 200 bullets made contact with 6 CDC buildings, hundreds of staff sheltered in place for hours. The intention is undeniable: this was an attempted massacre.
13.08.2025 19:59 —
👍 162
🔁 56
💬 3
📌 7
Just out in @agsjournal.bsky.social!
We developed and piloted an AI + care coach intervention to support ED-to-home transitions for people with dementia or cognitive impairment + their caregivers.
🧠↑ caregiver self-efficacy
📉↓ caregiver burden
Read more: doi.org/10.1111/jgs....
05.08.2025 14:15 —
👍 1
🔁 1
💬 0
📌 0

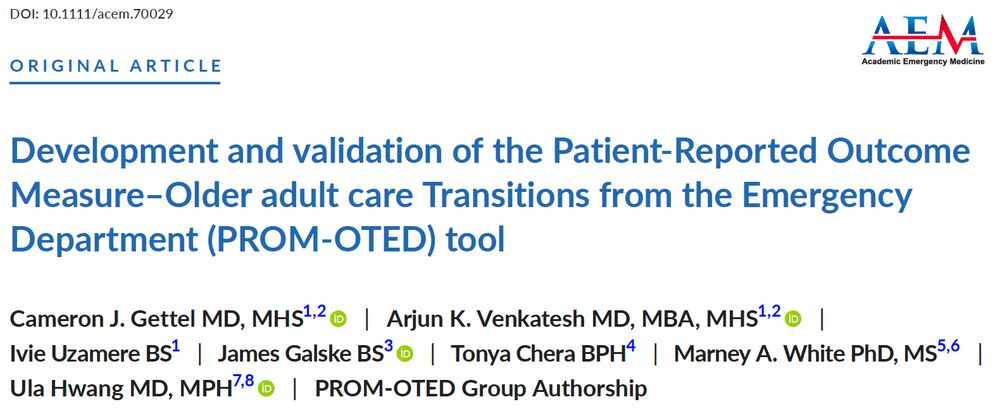
Congrats to @camerongettel.bsky.social @agem-saem.bsky.social on developing a new care transition measure for older emergency department patients! The PROM-OTED score!
#SAEM25 @saemonline.bsky.social
14.05.2025 19:41 —
👍 6
🔁 4
💬 1
📌 0

These emergency rooms adapt to the needs of older adults
Nobody wants to have to visit the emergency department, but "age-friendly" care seeks to make the experience safer for older people.
There's a trend to adapt #emergencydepartments to better meet the unique needs of our growing population of older adults.
Grateful to @ahascience.bsky.social and Mike Merschel for spotlighting this important shift!
#EMSky #GeriSky @acepnation.bsky.social
www.heart.org/en/news/2025...
06.05.2025 20:41 —
👍 7
🔁 4
💬 1
📌 0
I’m sorry for your loss Sarah - she sounds like an incredible woman and accomplished a great deal and positively influenced many lives in too short of a time
22.04.2025 03:11 —
👍 1
🔁 0
💬 1
📌 0
9/ @alzassociation.bsky.social @alzheimerssoc.bsky.social @istaart.bsky.social
#emergencydepartment #dementia #Alzheimers #cognitiveimpairment #EndAlz #medsky
21.04.2025 13:45 —
👍 1
🔁 0
💬 0
📌 0
8/ Bottom line:
✅ Screening for CI in the ED can work
🚫 Current diagnostic care transitions often break down
📈 Nearly 80% of those who followed up had confirmed CI
Let’s close the gap between detection and diagnosis - the ED can serve as a critical touchpoint.
21.04.2025 13:45 —
👍 1
🔁 0
💬 1
📌 0
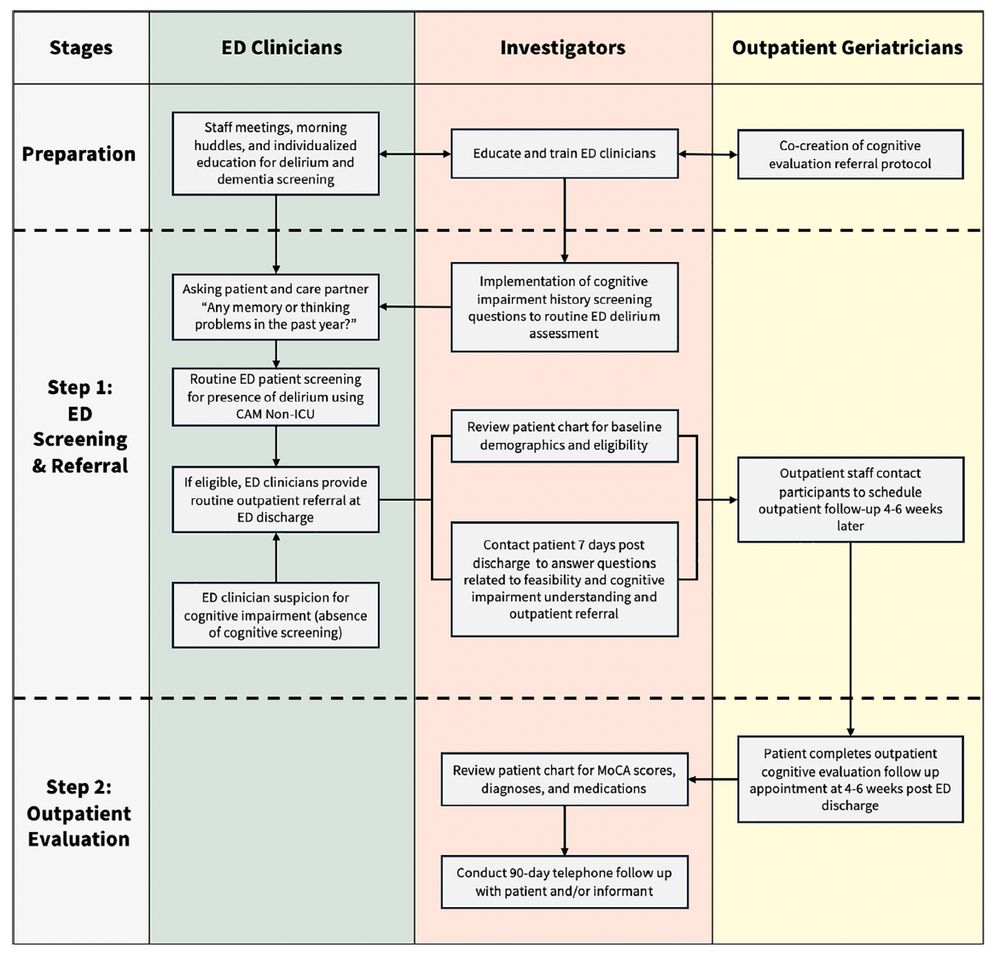
7/ We see real promise in pairing cognitive screening with EHR automation. Risk models, auto-referrals, and prompts could lighten ED workload and reduce missed diagnoses. Future work should explore AI and EHR-enhanced pathways. We’re just scratching the surface.
21.04.2025 13:45 —
👍 0
🔁 0
💬 1
📌 0
6/ What could help?
• Options like home-based evaluations
• Tech support (e.g., EHR-based alerts or automated referral prompts)
• Risk stratification to prioritize patients needing urgent follow-up
• Public health campaigns to reduce stigma and promote follow-up
21.04.2025 13:45 —
👍 0
🔁 0
💬 1
📌 0
5/ Why the referral and follow-up rates are suboptimal:
• Dementia stigma—patients/families may avoid referral
• ED teams overwhelmed
• Fragmented systems, no clear outpatient path
• CI may limit follow-up, esp. without care partner
• Unclear who’s responsible for post-discharge follow-up
21.04.2025 13:45 —
👍 0
🔁 0
💬 1
📌 0
4/ The problem: despite effective screening and high follow-up yield, most at-risk patients weren’t referred or didn’t follow up. A huge missed opportunity - EDs are often the first touchpoint for undiagnosed CI. Early detection → timely treatment, caregiver support, better outcomes.
21.04.2025 13:45 —
👍 0
🔁 0
💬 1
📌 0
3/ Of those 100 referred, only 19 completed an outpatient cognitive evaluation – again a big drop. Among them:
🧠 79% were diagnosed with some form of CI
🧠 63% had probable dementia
💊 Many were prescribed meds for CI, dementia, or depression.
When the ED refers and patients follow-up…it matters.
21.04.2025 13:45 —
👍 0
🔁 0
💬 1
📌 0
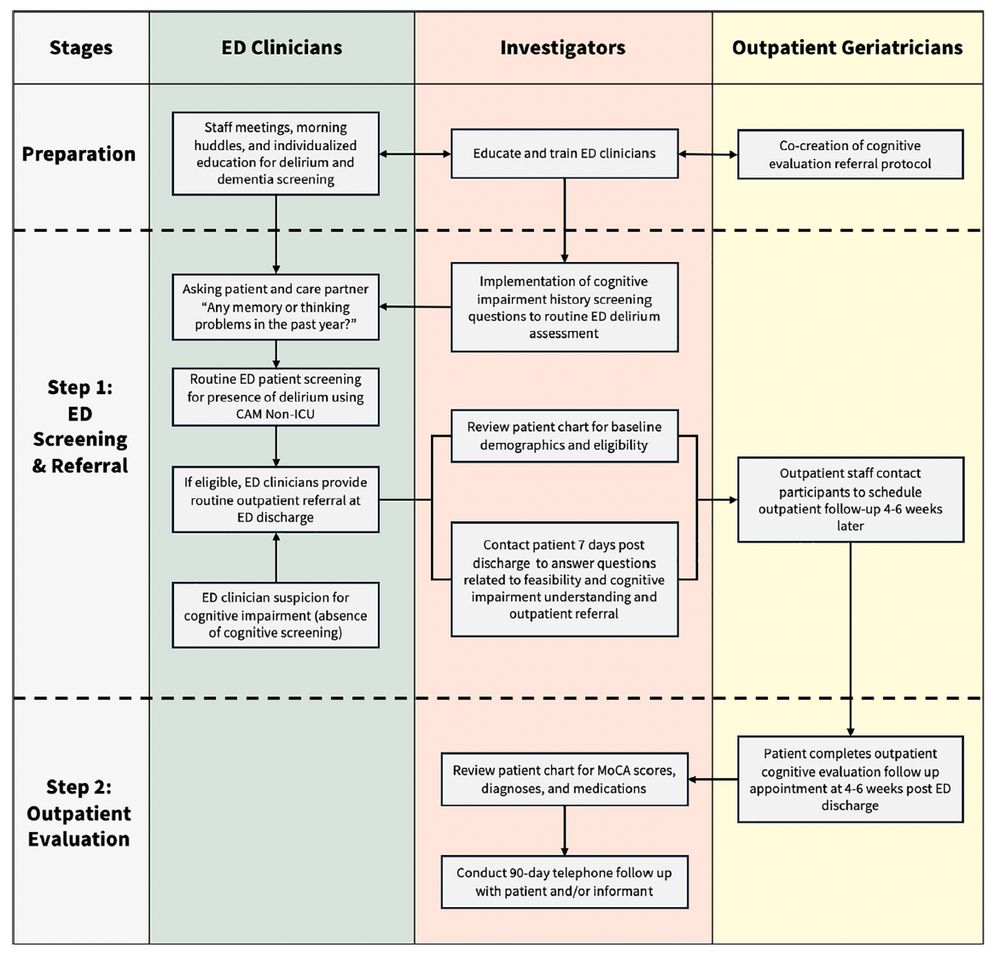
2/ First, we screened 9,359 older adults in the ED for memory/thinking problems. ~5% of patients and 33% of care partners flagged possible CI – 650 in total were eligible for referral. Yet only 100 were actually referred. That’s a big drop – we’ll get to potential reasons for this in a bit.
21.04.2025 13:45 —
👍 0
🔁 0
💬 1
📌 0
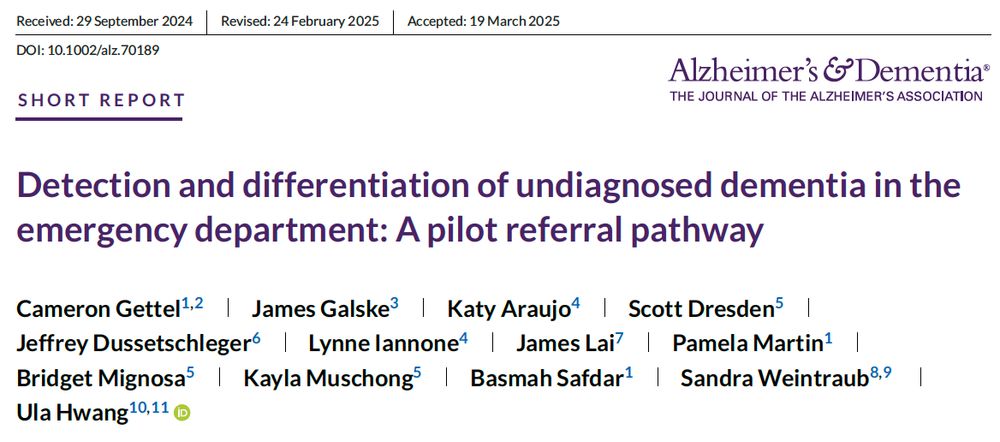
🧵 1/ Check out our team’s new study in @alzdemjournals.bsky.social on ED-based cognitive impairment (CI) screening and referral. What we found highlights both promise and pain points in real-world detection and follow-up for CI and dementia in the acute care setting.
bit.ly/4cMO8M0
21.04.2025 13:45 —
👍 6
🔁 2
💬 2
📌 0
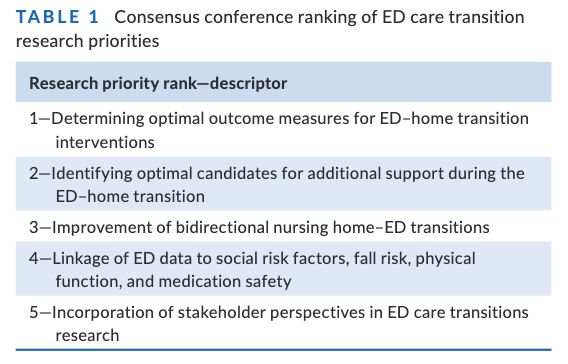
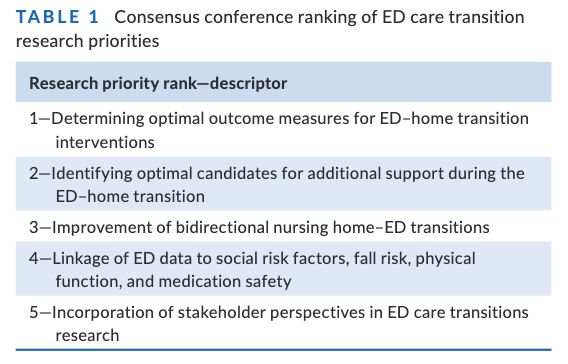
6/ This work is directly responsive to efforts from the multidisciplinary Geriatric Emergency care Applied Research (GEAR) network:
gearnetwork.org
pubmed.ncbi.nlm.nih.gov/34328674/
30.03.2025 20:00 —
👍 0
🔁 0
💬 0
📌 0
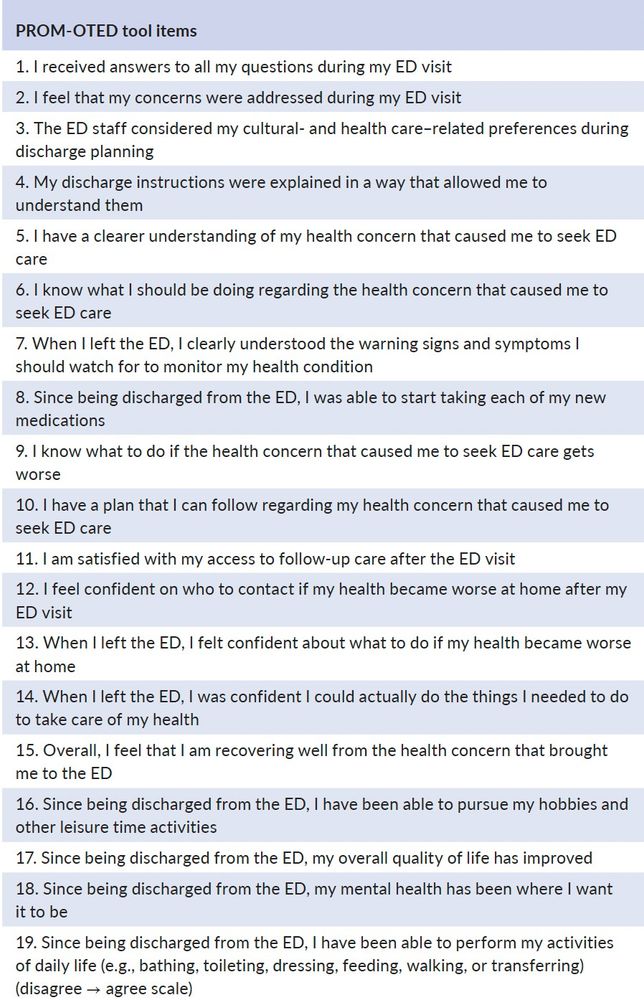
5/ 🏥 By providing insights into patients' perspectives on ED discharge and follow-up care, PROM-OTED can help health providers improve discharge processes and allow researchers to measure what matters to patients in future studies.
30.03.2025 20:00 —
👍 2
🔁 0
💬 1
📌 0
4/ ⏱️ With a mean completion time of just 5 minutes, the PROM-OTED tool can be administered via phone or electronically—making it feasible for diverse patient populations.
#GeriatricEmergencyMedicine #GeriEM #EmergencyMedicine #CareTransitions
30.03.2025 20:00 —
👍 0
🔁 0
💬 1
📌 0
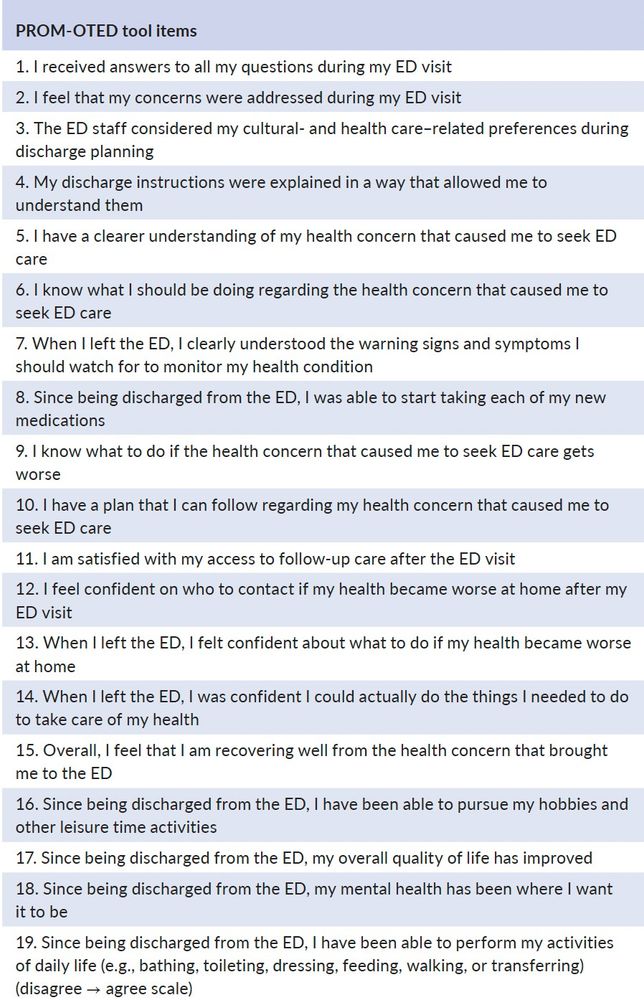
3/ ✅ The final 18-item PROM-OTED tool measures critical aspects like understanding discharge instructions, medication management, follow-up care, and quality of life. It’s validated with excellent reliability and a robust factor structure.
30.03.2025 20:00 —
👍 0
🔁 0
💬 1
📌 0
2/ 🧑🔬 Our study involved 290 older adults (65+) discharged from EDs over 3 years, using qualitative interviews, item generation, and psychometric testing to create a reliable measure of care transition outcomes post-ED discharge. #PatientReportedOutcomes #EDCare
30.03.2025 20:00 —
👍 0
🔁 0
💬 1
📌 0
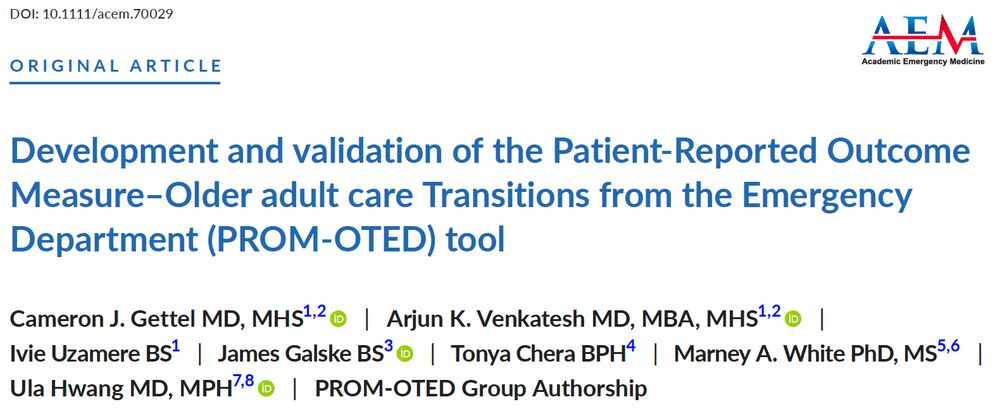
1/ 🚨 ED care transitions are critical for older adults, but no standardized tools have been available to measure patient-reported outcomes. Here we share the development and validation of the PROM-OTED tool to address this gap.
Access in @aem-journal.bsky.social: pubmed.ncbi.nlm.nih.gov/40155783/
30.03.2025 20:00 —
👍 5
🔁 2
💬 1
📌 0
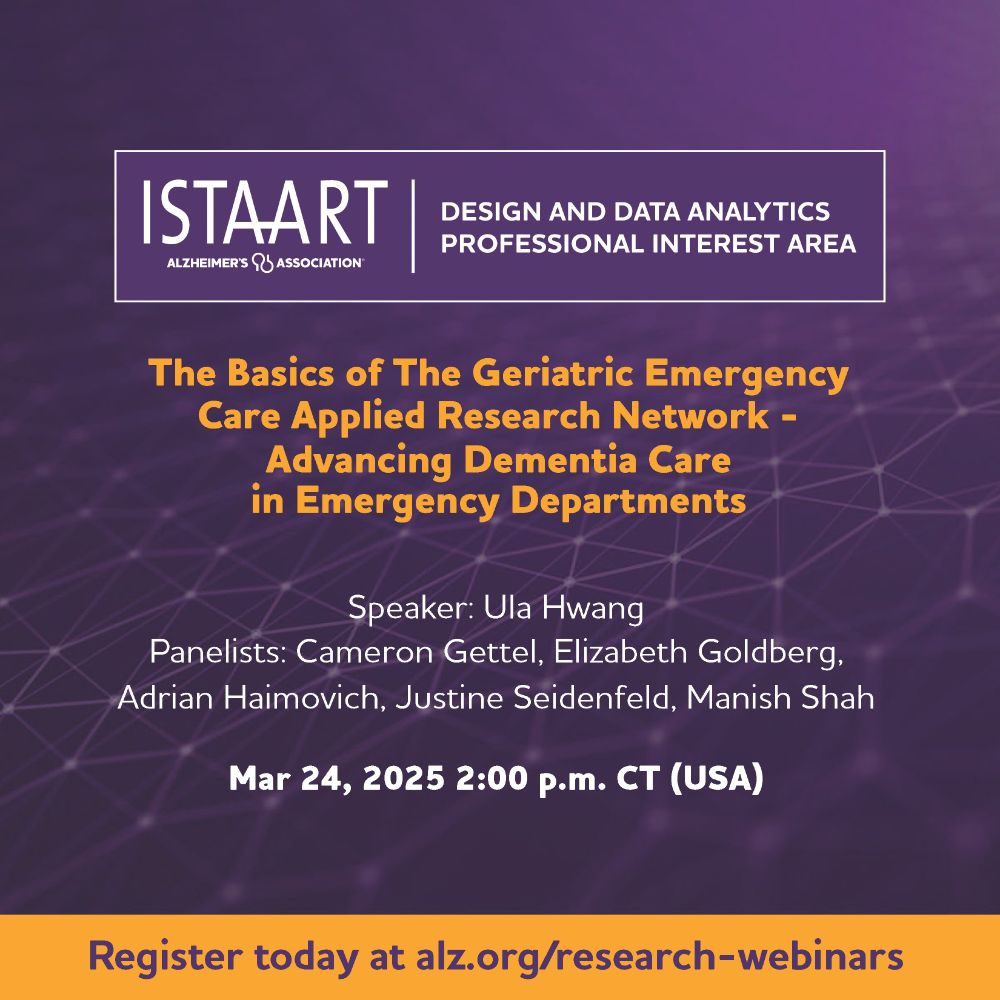
Grateful to present with @camerongettel.bsky.social @manish-shah.bsky.social & others on how we are improving #dementia care in the #emergencydepartment.
#Geriatrics #EMSky @agem-saem.bsky.social
Register here: alz-org.zoom.us/webinar/regi...
27.02.2025 16:02 —
👍 5
🔁 2
💬 0
📌 0
#alzsky #dementia #alzheimer #alzheimers #alz #sciencesky
30.01.2025 19:46 —
👍 0
🔁 0
💬 0
📌 0
10/ The big takeaway? Dementia care programs aren’t failing—they’re evolving. We must refine, target, & implement them better. GUIDE is an opportunity to learn from research & build a more effective, scalable system. Let’s get it right. 🚀🧠
30.01.2025 19:46 —
👍 2
🔁 0
💬 1
📌 0
9/ 🔹 D-CARE showed improved caregiver efficacy. GUIDE's focus on caregiver education & respite care may prove critical.
🔹 Hospitalizations & ED visits are modifiable. IN-PEACE showed this. A major reason to keep pushing for dementia-tailored care.
30.01.2025 19:46 —
👍 0
🔁 0
💬 1
📌 0
8/ 🔹 Targeting matters. Broad "one-size-fits-all" approaches may not work. Instead, models should be stepped, with different levels of care for early vs. late-stage dementia.
🔹 Implementation is key. Pragmatic trials are tough, esp. in COVID. GUIDE sites must be flexible & adaptive.
30.01.2025 19:46 —
👍 0
🔁 0
💬 1
📌 0
7/ Enter GUIDE, Medicare's new dementia care payment model launched in July 2024. It funds interdisciplinary teams, caregiver support, and 24/7 access to dementia expertise.
What should GUIDE take from D-CARE & IN-PEACE? 📌
30.01.2025 19:46 —
👍 0
🔁 0
💬 1
📌 0
6/ Subgroup findings suggest where dementia care can make an impact:
🔹D-CARE: Hints of benefit in caregiver self-efficacy in both intervention groups.
🔹IN-PEACE: Fewer ED visits/hospitalizations, esp. for African American patients & those with higher symptom burden.
30.01.2025 19:46 —
👍 0
🔁 0
💬 1
📌 0

Challenges and Innovations in Dementia Care
Dementia, a neurodegenerative disease characterized by progressive cognitive and functional loss, is a devastating illness that requires a complex set of medical and social services for care. It is al...
5/ A key issue brought up in the associated Editorial: Neuropsychiatric symptoms as a primary outcome. These are distressing but highly variable. Should we instead focus on outcomes like hospitalizations or nursing home placement?
bit.ly/4aDoHLI
30.01.2025 19:46 —
👍 0
🔁 0
💬 1
📌 0