


The annual #NephMadnessParty in Tromso, Norway 🥳 Between kidney cookies, rhubarb drinks, and licorice, we agreed that CAR-T is this year's #nephmadness winner 🏆 #arctic-cart
21.03.2025 19:19 — 👍 8 🔁 5 💬 0 📌 0@lbrinde.bsky.social
Kidney nerd in the Arctic! Associate Professor/Resident, University Hospital of North Norway/University in Tromsø Broad interests; from AKI and critical care to CKD and prevention. Biggest achievement: Top Resident Score #nephmadness 2024 🤓🏔️



The annual #NephMadnessParty in Tromso, Norway 🥳 Between kidney cookies, rhubarb drinks, and licorice, we agreed that CAR-T is this year's #nephmadness winner 🏆 #arctic-cart
21.03.2025 19:19 — 👍 8 🔁 5 💬 0 📌 0Very interesting! We seldom use vasopressin. However, we use dobutamine quite a lot. I guess this could be due to the cardiologist running the ICU. I still believe we could be more familiar with other vasopressors. Next time I consider using vasopressin, I will have your tips in mind 🙏
21.03.2025 09:39 — 👍 2 🔁 0 💬 1 📌 0I totally agree that RCTs are at the top of the pyramid and that we do not have evidence that vaso is better than NE/NA! But maybe the study indicates that we should use two vasopressors earlier? At which doses of NA do you start vaso? Btw, you are really inspiring!
20.03.2025 12:39 — 👍 3 🔁 0 💬 1 📌 0
NephMadness brackets
Very interesting regions indeed ajkdblog.org/2025/03/01/w...
#NephMadness #BlueRibbonFail incoming
Happy #NephMadness Day!
The 8 regions of #NephMadness 2025 have been revealed on the #AJKDBlog. If you're a #NephMadnessNewbie, we explain everything here: buff.ly/DCZDRfN
Looking forward to the fun and learning with all of you!

RESOLVE design: www.georgeinstitute.org/projects/ran...
11.02.2025 07:20 — 👍 5 🔁 1 💬 1 📌 0Thank you! I agree the DOPPS study has some bias. The small RCT by Paula et al (KI 2004) is interesting, showing decreased IDWG and fewer symptoms during HD. I wasn't aware of the RESOLVE study. Hope it provides answers! Meanwhile, we should individualize, but I will keep Na lower rather than higher
11.02.2025 07:34 — 👍 2 🔁 0 💬 0 📌 0
Check out the recent Cochrane review (behind a paywall…) if interested in dialysate sodium levels. They conclude that there is reduced interdialytic weight gain (IDWG) but more intradialytic hypotension. www.cochranelibrary.com/cdsr/doi/10....
10.02.2025 12:14 — 👍 1 🔁 0 💬 1 📌 0Preparing a presentation on HF in HD patients, focusing on sodium levels in dialysate. Low Na (<138) reduces IDWG and MAP, leading to decreased UF, which lowers the risk of intradialytic hypotension and myocardial stunning. What's the standard approach in #Nephsky: low or normal Na levels? #askrenal
10.02.2025 12:05 — 👍 2 🔁 3 💬 1 📌 0



Proposed age-adjusted eGFR thresholds for CKD 👇
#Nephpearls #NephSky
eGFR 75 for ages <40 years
eGFR 60 for 40-65 years
eGFR 45 for >65 years
👉 link.springer.com/book/10.1007...
👉 pubmed.ncbi.nlm.nih.gov/31506289/

Interesting! There are other studies reporting really good effect, such as this with 81 Chinese patients: karger.com/ajn/article-...
And this meta-analysis with 221 patients with MCD/FSGS: pubmed.ncbi.nlm.nih.gov/32293308/
However, I haven't found any studies assessing when to ✋ RTX
Gleder meg forresten til samarbeid i FuN! 😎
04.12.2024 21:44 — 👍 0 🔁 0 💬 1 📌 0It was about a year ago, but there were few/no side effects/complications of RTX, and the patient has been pleased with it. Anyway, I think I will reach the same conclusion as you. I will see if the attendees agree!
04.12.2024 21:42 — 👍 0 🔁 0 💬 0 📌 0Does anyone have experience with RTX in the maintenance treatment of steroid-dependent NS due to MCD/FSGS? 60-year-old 👴 with complete remission. Could stop prednisolone completely. Now, 4 rounds with RTX (6-month intervals). Is it safe to stop RTX and closely follow up? #askrenal
04.12.2024 15:07 — 👍 2 🔁 1 💬 3 📌 0Our group does research on the technique, and we were pleasantly surprised to find out it holds up in TR patients (paper coming soon!). Still big ? about cirrhosis, positive pressure ventilation, CKD/ESRD. And then there’s the issue that it was only really built to predict cardio renal aki.
04.12.2024 12:16 — 👍 3 🔁 1 💬 0 📌 0Very interesting! I will definitely check it out and follow your work closely. My conclusion is that we need several assessment tools to determine when the patient is in fluid balance.
04.12.2024 14:08 — 👍 0 🔁 0 💬 0 📌 0That's a valid point! I use vexus to supplement clinical examination, other types of pocus and medical history. So, I do not believe it is the “only and right answer.” What do you think? Which patients should we be more careful about assessing fluid status using Vexus?
04.12.2024 07:00 — 👍 0 🔁 0 💬 2 📌 0
Visual abstract of the BPROAD trial

Spanish version
The BPROAD visual abstracts are live
www.nephjc.com/news/bproad
Nice work from @kajareeg.bsky.social with Spanish version @dramiliflores.bsky.social
#NephJC #NephSky
Thank you! I guess there is a way to go, but it's nice to know that studies are ongoing. I hope and believe that complement inhibitors will be imported into LN in the future!
03.12.2024 20:34 — 👍 2 🔁 0 💬 0 📌 0

Vexus is a great tool when assessing fluid status in patients with CKD and heart failure. Today, we assumed that a 60-year-old 👵 had achieved dry-weight. However, vexus showed this! Now we are increasing the diuretics 💁 #pocus #vexus
03.12.2024 20:18 — 👍 7 🔁 2 💬 2 📌 0
➡️ Up next on #NephJC #NephSky 🦋
Join us for some high pressure discussion on Dec 3,4 as we discuss #BPROAD from #NEJM
nejm.org/doi/abs/10.1...
Tweetorial by @drpallaviprasad.bsky.social
So, the complement system plays a major role in lupus nephritis, and I know eculizumab can be effective in the ICU with LN flair. Is there any ongoing RCT investigating an oral complement inhibitor in LN? Could avacopan be an alternative to CNI or belimumab? C5a levels are up in sle #askrenal
02.12.2024 18:54 — 👍 3 🔁 1 💬 1 📌 0📌
23.11.2024 21:59 — 👍 0 🔁 0 💬 0 📌 0📌
19.11.2024 16:27 — 👍 0 🔁 0 💬 0 📌 0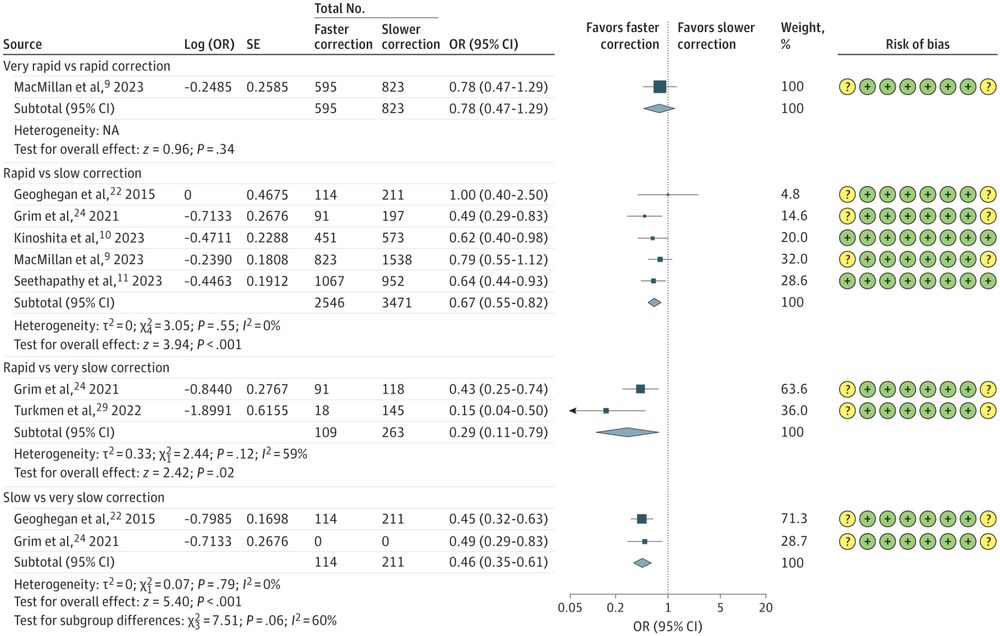
Honey, stop what you're doing, new hyponatremia research just dropped!
What's it say?
It looks like slow correction is associated with worse outcomes, like death and length of stay!
Was it just a small study?
No, it was a meta-analysis of almost 12,000 patients!
jamanetwork.com/journals/jam...
📌
18.11.2024 21:03 — 👍 1 🔁 0 💬 0 📌 0📌
18.11.2024 20:32 — 👍 2 🔁 0 💬 0 📌 0Agree! Observational data are really important and valid data 🙌 but how are you managing these patients? Affording to the RCTs such as BPROAD we should lower the target BP, also in older patients with diabetes, but the Veteran's study suggests the opposite🤔
18.11.2024 16:55 — 👍 0 🔁 0 💬 1 📌 0Achieved BP in the control group for BPROAD was 133. So it really did compare (nearly) guideline therapy vs even lower
"At 1 year, the mean SBP was 121.6 mm Hg (median, 118.3 mm Hg) in the intensive-treatment group and 133.2 mm Hg (median, 135.0 mm Hg) in the standard-treatment group."