

Happy 4th!
#nephbbq


Happy 4th!
#nephbbq
@schaeffer.usc.edu @keck.usc.edu
18.06.2025 19:55 — 👍 0 🔁 0 💬 0 📌 0
For my commentary on this very insightful study @JAMANetworkOpen
, link here: jamanetwork.com/journals/jam...
The study itself is here: jamanetwork.com/journals/jam...
@KeckMedicineUSC
@USCSchaeffer
Fin/
8/ Most importantly, we still don't know whether dialysis patients are helped or harmed by MA.
Unfortunately, our healthcare system isn't organized to put patient interests first. This study was a very interesting glimpse into how patients are ignored.
7/ Third, I worry that focusing on MA plans ignores the clear financial incentive that dialysis organizations have to steer patients into MA plans
And that dialysis organizations have way more power to influence patients than MA plans
6/ Clinicians were alarmed - Add this to a deluge of evidence that business interests are running away from clinicians to the potential detriment of patients
Clinician leaders ARE an important bulwark, and we should be wary of ignoring the professionalism of clinicians
5/ What are my additional takeaways from this interesting study?
First, it's important to recognize that MA is a story of heterogeneity - the large dialysis organizations are profiting heavily, but are the smaller ones? I'm not so sure
4/ Steering patients into MA is a no-brainer given how profitable it is
MA plans are profiting heavily as are dialysis organizations
3/ The authors found broad agreement that advertising could be misleading, false, and/or overwhelming
In some cases, participants described behavior that is hard to interpret as anything other than a bribe to induce MA enrollment
(here, DO = dialysis organization)
2/ This study was very broad! They interviewed over 50 executives and staff from MA plans, kidney care management companies, and dialysis organizations
Although it is a real limitation that patient perspectives weren't included. Hopefully forthcoming in paper 2?

I had the privilege of writing a commentary in @jamanetworkopen.com
on this very interesting qualitative study re: Medicare Advantage advertising in dialysis
In short, the flurry of ads are often misleading to patients, and it's unclear if patients are shortchanged
🧵 1/
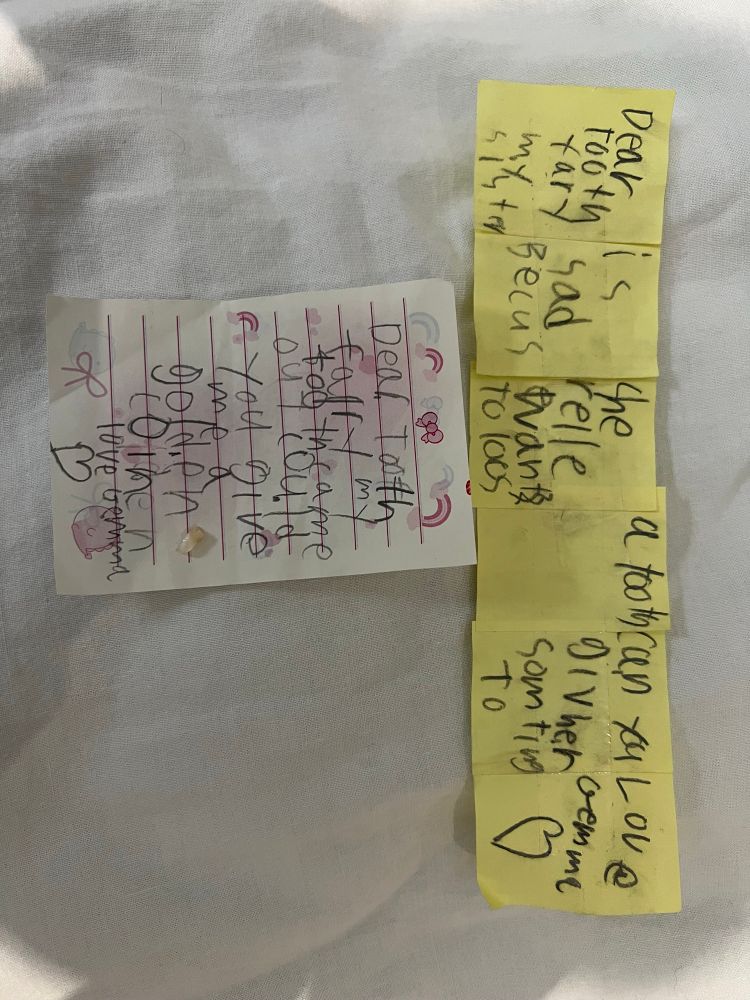
My daughter is too cute
28.05.2025 13:57 — 👍 2 🔁 0 💬 0 📌 0
How do out-of-pocket (OOP) costs at the point of pharmacy affect access to medications?
In a paper @JAMAHealthForum
(with Jillian Caldwell & others), we examine @CMSGov
TDAPA policy and show that it improved access to calcimimetics likely by reducing OOP
🧵1/ (LINK at end)


Nom nom nom
#nephbbq
Money shot below ⬇️
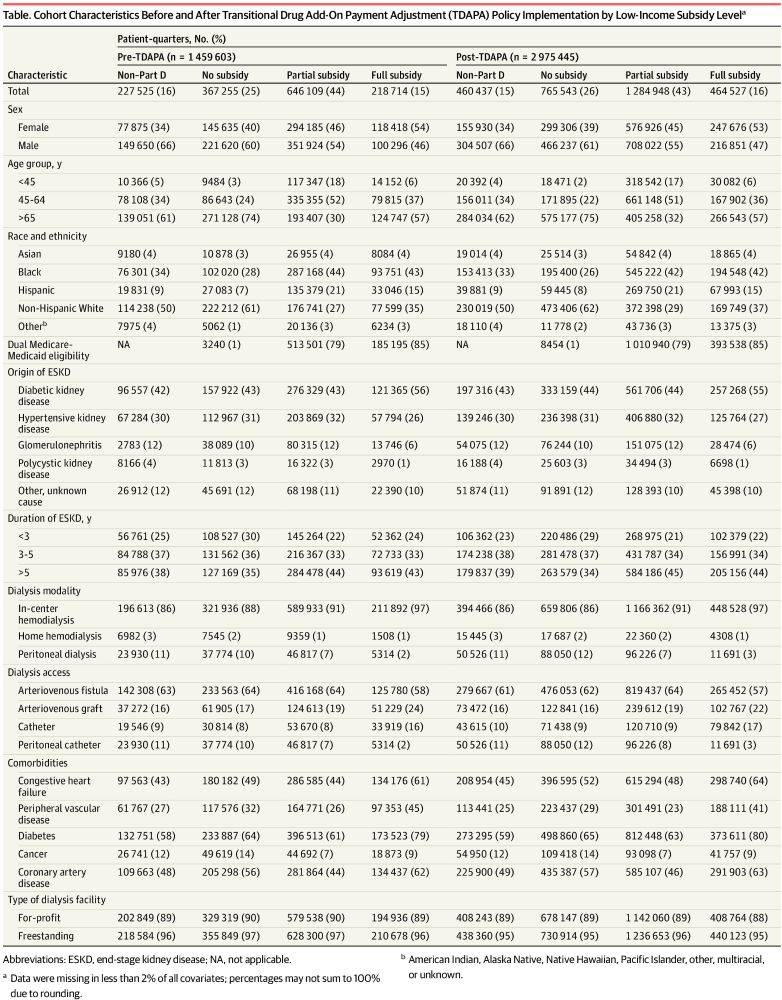
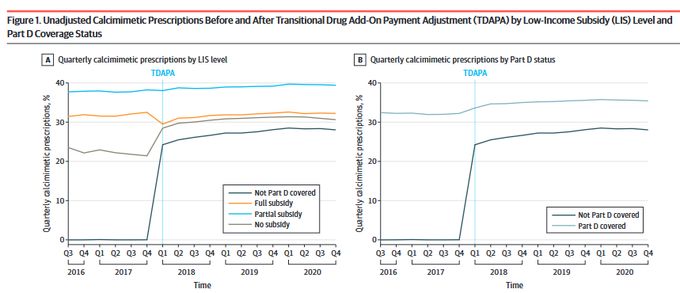
Compare to pts with FULL rx subsidies (who pay $0), pts with pts with Part D but NO subsidies had 10pp more rx fills, and pts with PARTIAL subsidies had 2pp more rx fills post-TDAPA.
i.e., the more you paid pre-TDAPA, the more meds you filled post-policy
Latest publication! 🚨
TL;DR:
1) MANY patients on dialysis pay high OOP costs for drugs 💸
-- nearly 20% have NO PART D plan
-- 25% have NO rx subsidies
2) Covering calcimimetics in Part B via TDAPA instead of Part D INCREASED rx fills 📈
Check out @eugelin06.bsky.social's 🧵 & our paper ⬇️
20% of patients dont have a prescription drug plan
I’ve yet to meet an esrd patient on zero meds
Shout out again @jilliancaldwell.bsky.social - she's a PHENOM and an all-star research fellow
This project wasn't easy: she stitched together multiple complex datasets and studied a very complex policy
I don't know when she's going on the market, but folks need to pay attention to her
Thanks to @jilliancaldwell.bsky.social who led this massive project and others @stanfordmedicine.bsky.social @schaeffer.usc.edu @keck.usc.edu
FIN
Tl;dr: TDAPA improved access to calcimimetics by improving prescription drug coverage
Read more @JAMAHealthForum
LINK: jamanetwork.com/journals/jam...
23/
I'm cautiously optimistic that this will IMPROVE access to phosphate binders, based on our historical experience with calcimimetics
22/

This doesn't just impact the past - this year, @CMSGov
was legislatively obligated to roll all phosphate binders (which are oral only) into the bundle. That is, binders are now in TDAPA
This came with some trepidation by industry and in some cases legal action
21/
In summary:
1) High OOP costs can prevent patients from getting their meds!
2) At least 20% of ESRD patients don't have a prescription drug plan, and >40% have no subsidies for copays
3) TDAPA is a reasonable mechanism to expand drug coverage
20/
Limitations cont'd
3) We didn't include outcomes (but will in future work)
4) The diff-in-diff estimator doesn't control for confounders that are not time invariant
5) technically, we violated the parallel trends (again they were small but statistically significant)
19/
Some limitations to our work
1) we could not observe unpaid prescription fills (i.e., did patients get calcimimetics through charity or pay 100% of list price?)
2) we only studied traditional Medicare and not Medicare Advantage
18/
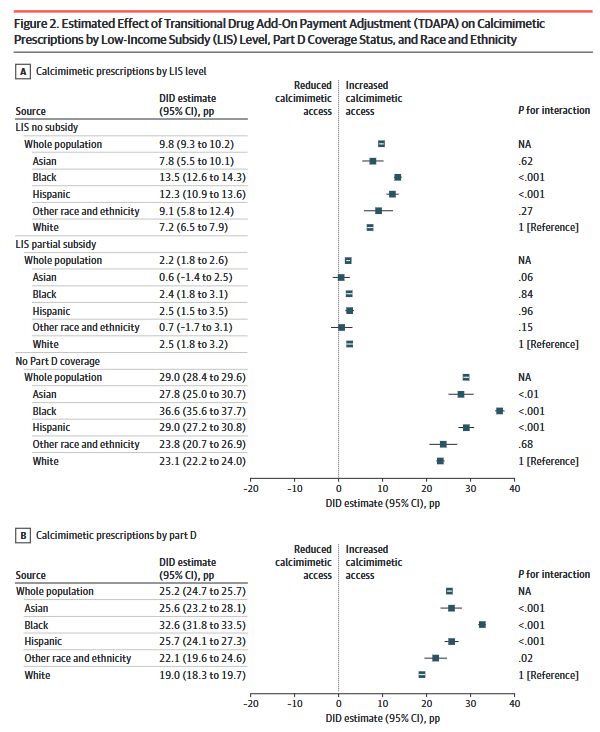
You can see the formal difference-in-differences (and triple differences) comparison in the following forest plot, with p-values for interaction
17/
One question is whether there was heterogeneity in the policy's benefit. And indeed we show that Black and Hispanic patients received the most benefit from the policy (for the nerds, we used a triple difference to do this)
16/
Some methodological notes
- it adjusts for UNOBSERVED time-invariant factors. So this quasi-experimental approach reduces time-invariant selection bias related to LIS coverage
- we technically violated pre-TDAPA parallel trends, but they were small relative to the effect
15/
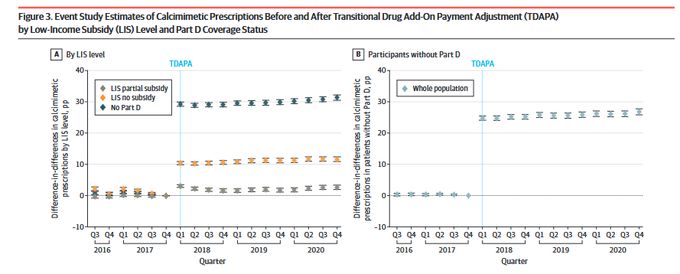
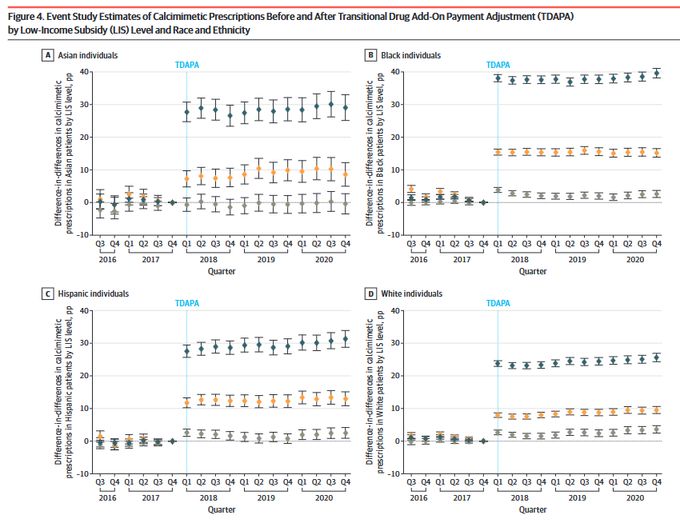
Using a difference-in-differences estimator (we used a 2-way fixed effects estimator in an event study), we show close to parallel trajectories among these 4 groups, but a relative increase in calcimimetic access, again based on the generosity of the subsidy
14/
So what were the overall trends in calcimimetic use?
Exactly what one would expect: large increases in calcimimetic use related to how generous the change was in drug coverage
Note, we saw a small decline among patients with the full subsidy
13/