MSN
Humans:
- Taking my job?
----- I hate AI!😡
- Helping me get rid of another human when doing something?
----- I love AI!🥰
We are doomed!!
www.msn.com/en-us/health...
02.10.2025 11:40 — 👍 2 🔁 0 💬 0 📌 0

Disseminating innovations in health care - PubMed
Health care is rich in evidence-based innovations, yet even when such innovations are implemented successfully in one location, they often disseminate slowly-if at all. Diffusion of innovations is a m...
The recipe includes: trust, incentives, visible early adopters, and leadership.
Innovation only starts at invention. Adoption is the next main component.
How many clever solutions do you know that need a push towards adoption?
Here is the JAMA article again: pubmed.ncbi.nlm.nih.gov/12697800/
28.09.2025 18:11 — 👍 0 🔁 0 💬 0 📌 0
The lesson? Discovery is only half the battle.
Without systems that support diffusion, life-saving interventions stay stuck in labs and journals instead of reaching patients.
28.09.2025 18:11 — 👍 0 🔁 0 💬 1 📌 0
In healthcare today, effective interventions (drugs, vaccines, care models) take DECADES to become routine.
Innovation diffuses slowly even when the benefits seem obvious.
28.09.2025 18:11 — 👍 0 🔁 0 💬 1 📌 0
"To introduce any new article of food among seamen... requires both the EXAMPLES and the authority of a Commander."
- Captain James Cook.
LEADERSHIP DRIVES DIFFUSION!
28.09.2025 18:11 — 👍 0 🔁 0 💬 1 📌 0
EVIDENCE ALONE IS NOT ENOUGH!
Adoption required authority, leadership, and culture change.
Cook saw this and he benefited from the immediate application for himself and his crews.
28.09.2025 18:11 — 👍 0 🔁 0 💬 1 📌 0
However, it wasn't until 1865 - 264 yrs after Lancaster, that the British Board of Trade required merchant ships to follow suit.
Two and a half centuries from proof to policy!!! So why so slow?? 😵💫
28.09.2025 18:11 — 👍 0 🔁 0 💬 1 📌 0
It took 48 more years for the British Navy to officially issue citrus rations.
Scurvy nearly disappeared from its fleets.
28.09.2025 18:11 — 👍 0 🔁 0 💬 1 📌 0
Year: 1747 (146 years later!)
James Lind repeated the test aboard HMS Salisbury.
Again, citrus worked!! Now, there should be immediate adoption, right? Again, not even close!!😢
28.09.2025 18:11 — 👍 0 🔁 0 💬 1 📌 0
Year: 1601. Nobody knows about vitamin C at that time.
Captain James Lancaster tested lemon juice at sea.
👉 His sailors remained healthy. 🎉💪
👉 All while almost HALF the crews on other ships died of scurvy.💀
You'd expect immediate adoption? Not even close. The Navy ignored it.
28.09.2025 18:11 — 👍 0 🔁 0 💬 1 📌 0
15 L interdialytic wt gain.
Record?
Pt was trying to beat nausea with chips and water.
03.09.2025 20:49 — 👍 0 🔁 0 💬 0 📌 0

How are our patients dealing with these tremendous costs?
Do you have ppl in ur clinic to help pts obtain these medicines at an affordable cost?
Source: Primer on Diabetes Management www.vumedi.com/video/primer...
02.09.2025 00:46 — 👍 2 🔁 0 💬 1 📌 0
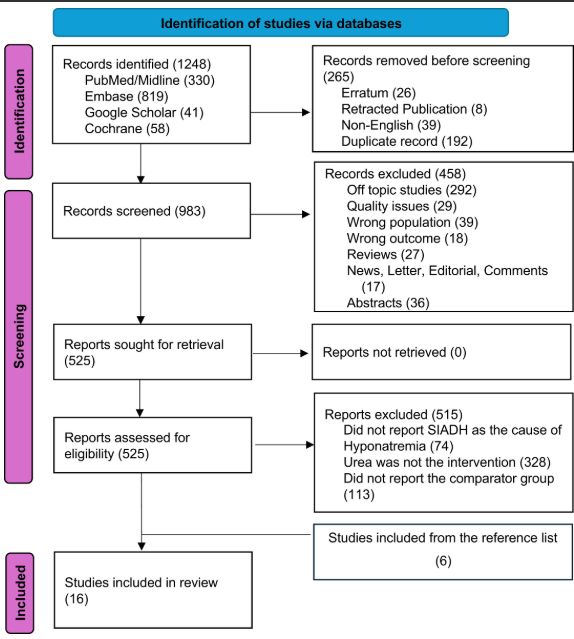
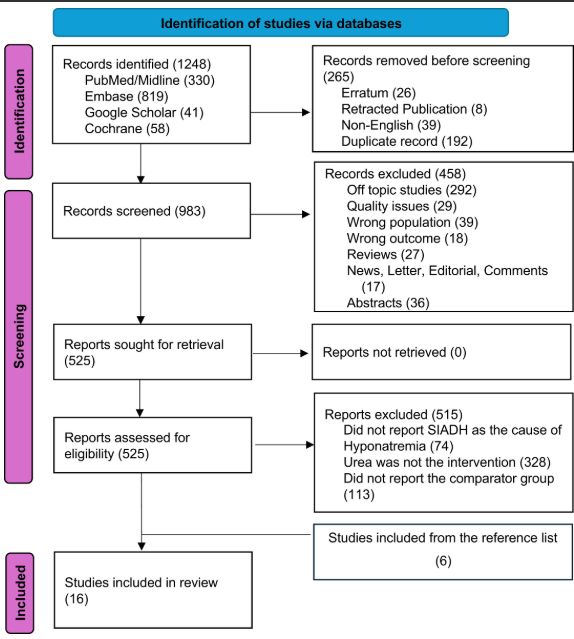
In case you missed it on the #AJKDBlog:
AJKDBlog Interviews Editor Timothy Yau caught up with Dr. Subhash Chander to discuss if urea is effective for managing SIADH-induced hyponatremia.
bit.ly/ChanderBlog25 (FREE)
03.08.2025 16:01 — 👍 3 🔁 1 💬 0 📌 0
Do u have a local policy for picc- and mid-lines for pts with renal impairment?
🧭 Any simple algorithm that can be shared with other specialties?
⛔️ “Has to be discussed with nephrology” is a battle- we r the bad people who r inconsiderate of realities of the pt’s (immediate) care!
#askrenal
25.07.2025 19:21 — 👍 2 🔁 1 💬 0 📌 0
a good biomarker of what? 😊
Diet? Inflammation? Liver disease? Kidney disease? (Example etiologies)
High risk patients for mortality or other poor outcomes? (outcomes)
Not good as in non specific: yes.
But good as gold as risk marker.
23.07.2025 01:25 — 👍 2 🔁 0 💬 1 📌 0
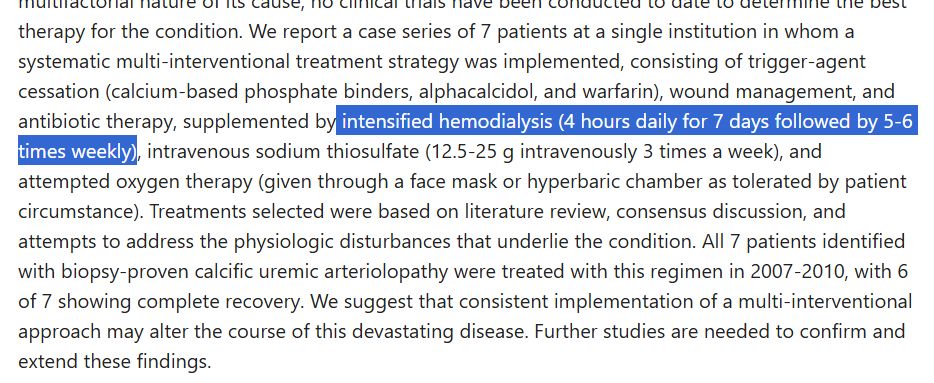
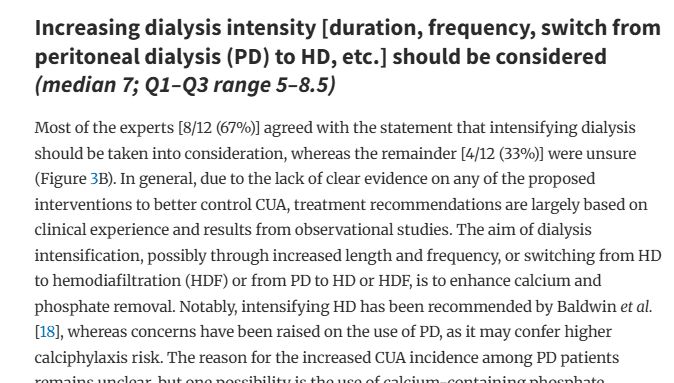
⚠️ Calciphylaxis is a debilitating and painful condition that is hard to treat.
▶️ Do you use daily dialysis as part of treatment? If so, what criteria do you use?
#askrenal
pubmed.ncbi.nlm.nih.gov/21872378/
doi.org/10.1093/ndt/...
22.07.2025 03:23 — 👍 4 🔁 4 💬 1 📌 0
*screaming
20.07.2025 02:32 — 👍 1 🔁 0 💬 0 📌 0
I once witnessed a cardiothoracic surgeon (aka God) SCREENING in ICU: “I WANT DIALYSIS”
for a patient after he was told nephrology suggested a different plan. 😬😟
19.07.2025 23:44 — 👍 7 🔁 0 💬 2 📌 0
There are gaps in the evidence, particularly for whether interventions to increase alb directly lower the risk of adverse outcomes.
19.07.2025 23:38 — 👍 2 🔁 1 💬 0 📌 0
Treatment should target underlying causes of low alb rather than the lab values alone. Eg protein-energy wasting (PEW), chronic inflammation, poor dietary intake, and comorbidities (including infections and chronic inflammatory conditions).
+ nutritional interventions and tailored dietary plans.
19.07.2025 23:35 — 👍 2 🔁 0 💬 1 📌 0
The relationship persists even after adjustment for comorbidities, inflammation, and nutritional status, indicating low albumin is an independent prognostic *marker*, and not just a surrogate for underlying disease severity or acute illness.
19.07.2025 23:21 — 👍 2 🔁 1 💬 2 📌 0
Yes. The association has been reported in multiple populations, including hospitalized, acutely ill, and community-dwelling individuals. Eg, albumin < 37 g/L is associated with up to a two-fold increase in long-term mortality even after adjustment for other risk factors.
19.07.2025 23:21 — 👍 2 🔁 0 💬 1 📌 0
YouTube video by The Late Show with Stephen Colbert
Stephen Colbert Announces The Cancellation Of “The Late Show”
That’s sad. I never imagined it would happen.
youtube.com/watch?v=AuqE...
18.07.2025 03:24 — 👍 0 🔁 0 💬 0 📌 0
Is it just me or is it really awkward?
".. and they are all known as non-steroidal anti-inflammatory drugs, or NSAIDs".
I am sure I lose patients at "non-ster.."!
How do you tell ur pts about them?
16.07.2025 21:52 — 👍 0 🔁 0 💬 0 📌 0
“Does not smoke, drink, or work”
Made my day 😂
15.07.2025 21:49 — 👍 1 🔁 0 💬 0 📌 0
Practical handbook of kidney diseases. Just-in-time information when and where you need it. https://apple.co/454QweZ. Editors: Mark Rosenberg & Sandeep Gupta
Democratic Nominee for Mayor of NYC. Assemblymember. Running to make this city affordable. Democratic Socialist. Early Voting: 10/25 - 11/2. Election Day: 11/4. zohranfornyc.com
A nephrologist based at Medical University of Białystok, book lover. Here because medicine is fun 🤩.
Welcome to the official Bluesky account for Kidney International!
The Official Journal of the International Society of Nephrology
@ISNKidneyCare
https://www.kidney-international.org/
I am a previous dialysis person & 3rd generation kidney failure member of my family. I received a deceased donor kidney transplant almost 9 years ago.
Wife, mom, nephrologist. Passionate about taking care of the whole person and goal directed based therapy. Lover of sarcasm and hockey and pro cycling.
no man is an island.. an italian nephrologist living and working in barcelona. Medicine, food, and sports are my interests
Top news and commentary for technology's leaders, from all around the web.
This account shares top-level Techmeme headlines. Visit https://techmeme.com/ for full context.
Showcasing the latest in kidney care, research, and innovation. Follow for updates from ASN publications, including JASN, CJASN, Kidney360, and Kidney News.
Infectious Disease Epidemiologist investigating #AMR ~ Based at The Kids Research Institute Australia.
Interest in Australian politics and global affairs.
Servant to two Lebanese ex-street cats
reposts ≠ endorsement
https://orcid.org/0000-0002-5295-8451
I’m the free, easy-to-use tool that helps you collect, organize, annotate, cite, and share your research sources.
Nephrology I Epidemiology I Biomarkers I Uromodulin I ADPKD I PAD I Powerlifting. CHCF Fellow. All activities = personal opinions.
NYU Langone Health, Department of Nephrology
Independent, board-certified patient advocate since 2014. Helping people find the health care they need at a cost they can afford.
Former medical video writer/producer in Texas Med Center. Based in Houston, TX.
Nephrologist. Views are my own. #UrinarySediment #Hyponatremia #POCUS
👉 www.swissnephro.org