



Dr Bilgili showed us the outcomes after OHTx divided by need of ECMO at 72 hours post surgery. ECMO need at 72 hours greatly worsens survival.
30.04.2025 17:58 — 👍 2 🔁 0 💬 0 📌 0@drmatteofabbri.bsky.social
Cardiology fellow at Inova. My opinions are my own. He/Him. BLM. Passionate about heart failure and pulmonary hypertension. ❤️




Dr Bilgili showed us the outcomes after OHTx divided by need of ECMO at 72 hours post surgery. ECMO need at 72 hours greatly worsens survival.
30.04.2025 17:58 — 👍 2 🔁 0 💬 0 📌 0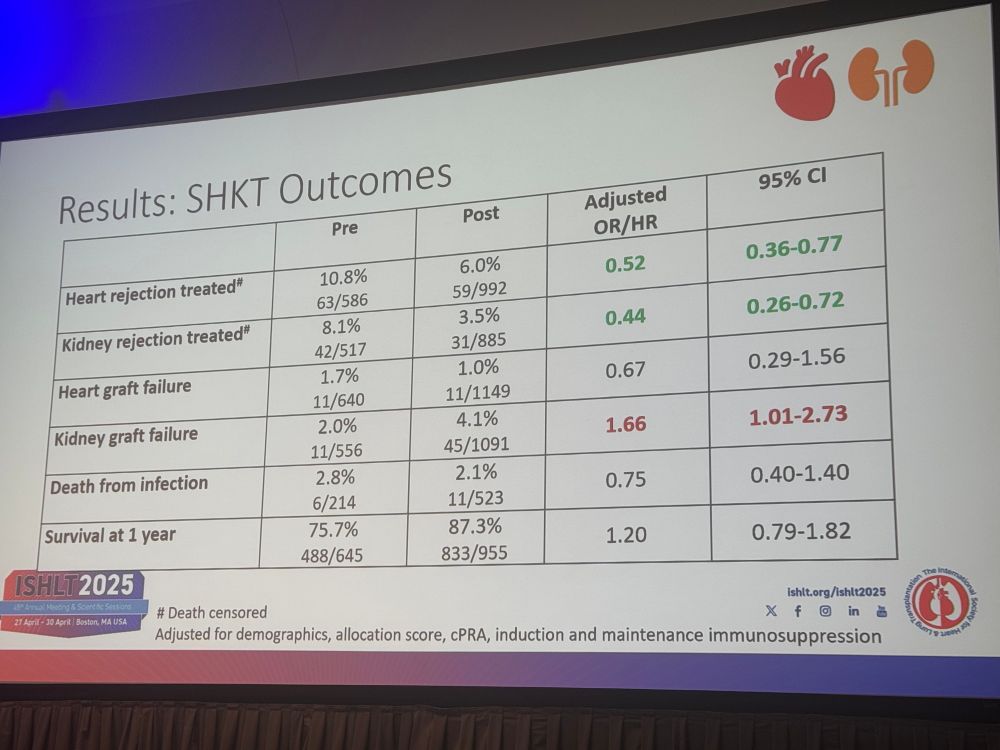



Dr Huang shows pre and post allocation change status change in immunosuppression and outcomes among multi-organ transplant.
Super interesting data. @ishlt.bsky.social #ISHLT2025




Dr Elbert Heng shows amazing study on survival of patients with ACHD receiving OHTx vs multiorgan transplant alone.
❤️ and 🫁 carry the worse survival so far.
@ishlt.bsky.social #ISHLT2025




Dr Paula Ramirez shows us their new predictive models to discriminate if ❤️ and kidney transplant is superior to kidney after ❤️. Beautiful work which can help change clinical practice at #ISHLT2025 @ishlt.bsky.social
30.04.2025 17:22 — 👍 1 🔁 0 💬 0 📌 0



Amazing work presented from Dr Topkara who developed a kidney risk score which predicts the risk for AKI/HD after ❤️ transplant! High AUC, higher than eGFR alone!
#ISHLT2025 @ishlt.bsky.social

Dr Hussain showed us a single center experience of Fontain patients receiving ❤️ transplant. Should they get a liver as well? Seems like all 24 of them had recovery of the liver function after transplant without needing a a new liver.
Great science at #ISHLT2025 @ishlt.bsky.social




Finally we talk about induction with Dr Barten. To induce or not to induce? This is the dilemma!
And Dr Carboni showed us how AI can be implemented in helping us with HLA matching.




It’s AB0ut time we talk with Dr Aversa about AB0! Super interesting case of an 0 patient receiving nonA1 🫁 transplant with no signs of rejections.
Incredible science showed at #ISHLT2025 @ishlt.bsky.social




Followed by Dr Guillaime Coutance guiding us through PRAs. Which antibodies should we look for and how to measure???
Dr Lyster showed us what to do with highly sensitised patients pre and post transplant.
#ISHLT2025




And last day at #ISHLT2025 we go through the consensus statement with Dr Annette Jackson. Amazing talk on the use of antibodies in transplant.
@ishlt.bsky.social

Did you get the reference?
29.04.2025 14:33 — 👍 0 🔁 0 💬 0 📌 0
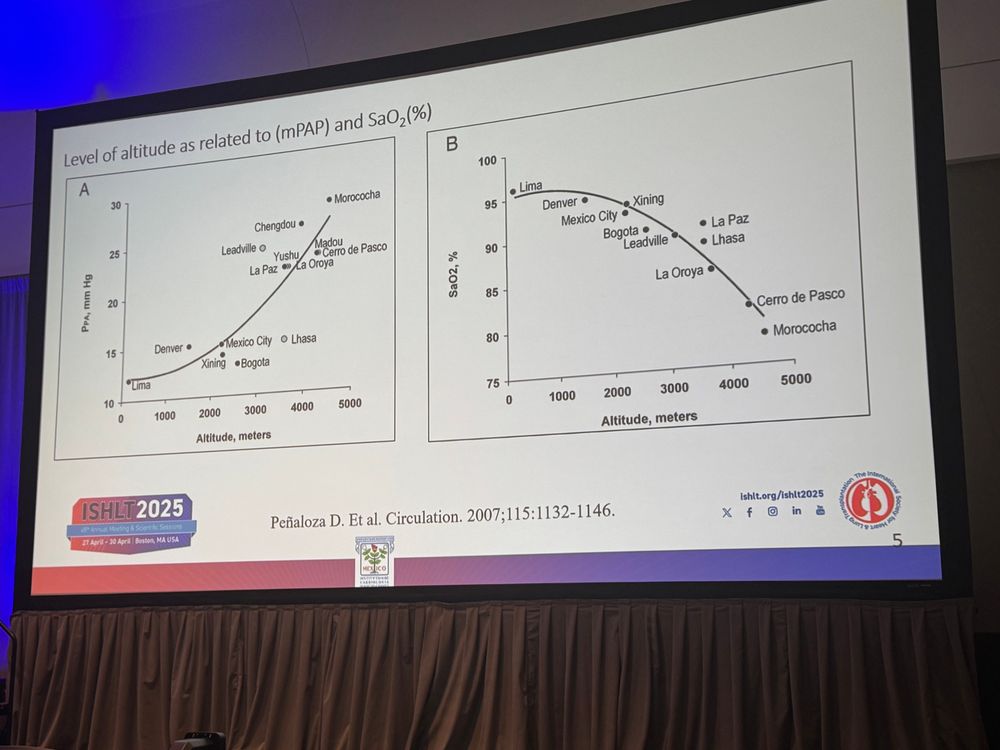


🎯 Dr. Tomas Pulido presented Out of the woods: High-altitude PAH. This subset of PAH is seen frequently in certain areas of south America and tend to improve with meds and moving to low altitude areas.
29.04.2025 14:32 — 👍 0 🔁 0 💬 0 📌 0



🎯 Dr Valentina Stosor presented Shake it Off: HIV associated PAH. HIV infection induces changes in the PA other than from direct infection. Drugs interactions are frequent between PA vasodilators and ART.
29.04.2025 14:30 — 👍 0 🔁 0 💬 0 📌 0



🎯 Dr Camila Loureiro presented I forgot that you existed: Schistosomiasis-Associated pulmonary arterial hypertension. Schistosoma is extremely frequent in certain areas of Africa, Asia and Brazil. We dipped dig on the treatments and diagnosis of such a rare subset of disease.
29.04.2025 14:29 — 👍 0 🔁 0 💬 0 📌 0



🎯 Dr Hooman Poor presented Bad Blood: Pulmonary Hypertension, Hematologic disorder and Bone Marrow Transplant. Sickle cell, dasatinib associated PAH and mieloproliferative disease
29.04.2025 14:27 — 👍 0 🔁 0 💬 0 📌 0



🎯 Dr Arun Jose presented: When the liver is the source of evil: porto-pulmonary HTN and liver transplantation.
PoP-PH is different from Hepato-pulmonary syndrome, which tends to regress after liver transplant. Liver transplant can improve PoP-PH though PH can persist.
This morning at ISHLT I’m sensing a theme, let’s see if any of you catch on that. Rare causes of PH.
@ishlt.bsky.social
#PAH
#PH
#Rightventricle
#rare




🎯 Dr Arun Jose presented: When the liver is the source of evil: porto-pulmonary HTN and liver transplantation.
PoP-PH is different from Hepato-pulmonary syndrome, which tends to regress after liver transplant. Liver transplant can improve PoP-PH though PH can persist.

We finish with a great talk from the amazing @nickbruin.bsky.social about the Delphi consensus.
Refer early and often
Reassess your patient. 🫁 transplant save lives and improves quality of life in PAH
#PAH #PH #lungtransplant #ISHLT2025
@ishlt.bsky.social
onlinelibrary.wiley.com/doi/full/10....



What is the role of MCS in PAH and cardiogenic shock?
1) patient selection
2) choose the RIGHT access
3) have an exit strategy in view
4) start PH therapies
5) consider transplant
These are few of the points we discussed today with Dr Sommer @ishlt.bsky.social
#ISHLT #PAH #PH




What can you do when a patient with PH land in the ICU with Shock?
Dr Mads Andersen walks us through
Preload treatment
Inotropes and its use
Afterload for PH
Important talk @ishlt.bsky.social #ISHLT2025 #PH

And from the Right Ventricle- Right atria interaction we move to the complex relationship between heart - kidneys and lungs in PH with an amazing talk from Dr. Rosenkranz.
#ISHLT2025 #PAH #PH
@ishlt.bsky.social
Today we dig deep in the pathophys of PH #ISHLT2025 with Dr Frances De Man on pressure loop of the RA.
Super interesting discussion on what happens to myocites in the right atrium.
@ishlt.bsky.social #PAH #PH

We finished with Dr David Jenkins and CTEPH talks.
When confirmed CTEPH we should ask:
🟢is patient operable? If YES PTE
NO?
🟢Can we do BPA?
NO?
🟢Riociguat
New direction? Can we combine such treatments for high risk patients?

We also talked about group 3 PH with Dr Shlobin Oksana. The different pathophysiology of it and possible treatment options.
Differentiate between:
🟢COPD-PH
🟢CPFE-PH
🟢ILD-PH
More studies are needed with better characterisation of PFTs for therapeutic target.

We also talked with Dr Jessica Huston about PH in LHD (group 2).
Zone of uncertainties (PCWP 12 - 18) use other modalities to help with the diagnosis like echo etc.
Think about PH-LHD in stages:
A at risk
B structural heart disease
C symptomatic patient
D predominant RVF

Following @ChristianGerges summarised the treatment of PAH and the new algorithm.
🟢 not high risk start with dual oral therapy
🔴High risk: triple therapy up front with IV prostanoids
Frequent re-assessment is key with uptitration of therapy to achieve a low risk profile.

First, we started with a great talk from @RaymondBenzaMD talking about updates on classifications, zone of uncertainties as well as risk stratification tools.
Briefly:
🟢 Mean PA > 20 mmHg defines PH (previously 25 mmHg)
🟢 PVR > 2 WU
🟢 genetic testing
🟢 think about drugs

Today @ishlt.bsky.social in Boston we talked about Pulmonary Hypertension.
Here the main take-away from the Updates on the 7th World Symposium.

In people with diabetes, GLP-1 and SGLT2i drugs were associated with less Alzheimer's disease and related dementias
jamanetwork.com/journals/jam...